Ultraviolet B (UVB) phototherapy is an advanced treatment modality used to manage various skin conditions, including psoriasis, atopic dermatitis, and vitiligo. This therapy utilizes shortwave ultraviolet radiation to suppress DNA synthesis, thereby reducing inflammation and improving skin health. Recent advancements have made narrowband UVB phototherapy (311–312 nm) a preferred choice over broadband UVB phototherapy (270–350 nm), owing to shorter exposure times and extended periods of remission.
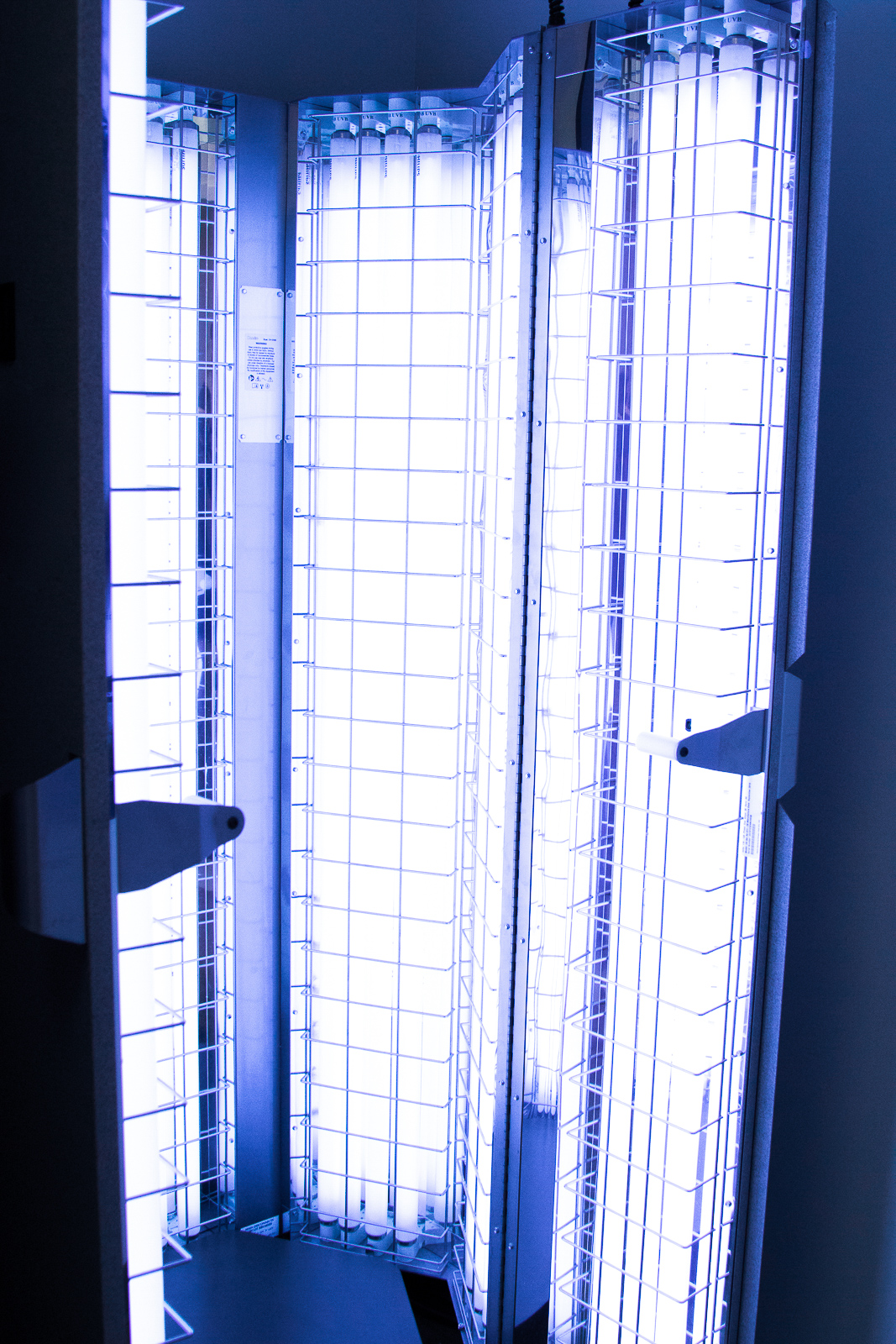
UVB phototherapy is administered in a specially designed cabinet equipped with fluorescent light tubes. These tubes emit targeted ultraviolet radiation to treat specific areas, such as the hands or feet, or provide full-body coverage. During full-body treatments, patients must undress, covering the genitalia, and protect their eyes or faces using goggles or masks to prevent unintended UV exposure.
Treatment frequency typically involves three sessions per week, spaced at least 24 hours apart. Each session begins with short exposure times, usually under five minutes, which may gradually increase to a maximum of 30 minutes, depending on individual tolerance and response. The duration and number of sessions are tailored to the patient’s skin type, condition, and treatment history. Prior to starting treatment, phototesting is conducted to determine the minimum erythemal dose (MED), which is the smallest UVB dose that causes skin redness. Therapy often starts at 70% of the MED, with incremental increases of 20% per session, provided there are no adverse reactions.
In addition to full-body treatments, targeted phototherapy devices, such as excimer lasers and UV combs, are available for treating difficult-to-reach or localized areas, minimizing exposure to unaffected skin.
UVB phototherapy is effective in managing a range of dermatological conditions:
- Common Indications: Psoriasis, atopic dermatitis (eczema), and vitiligo are the primary conditions treated with UVB phototherapy.
- Other Indications: The therapy also benefits patients with nodular prurigo, cutaneous T-cell lymphoma, pityriasis lichenoides, dermographism, lichen planus, mycosis fungoides, polymorphic light eruption, cutaneous graft-versus-host disease, mastocytosis, and generalized pruritus.
Psoriasis:
Psoriasis, a chronic inflammatory skin condition, often responds well to UVB phototherapy. Most patients experience significant improvement or complete clearance after 12 to 24 treatments. Remission periods can last for months, though maintenance treatments may be necessary for recurrent flare-ups.
Dermatitis:
For severe cases of dermatitis, particularly atopic dermatitis, UVB phototherapy can offer relief. Treatment regimens for dermatitis often require longer sessions and extended courses compared to psoriasis.
Vitiligo:
UVB phototherapy is particularly effective in vitiligo, as it suppresses immune responses and stimulates cytokines to promote repigmentation. Treatment is administered twice weekly for three to four months and may extend to one or two years, depending on progress. However, caution is advised for individuals with fair skin due to potential side effects.
While UVB phototherapy is generally safe, certain conditions contraindicate its use:
- Absolute Contraindications: These include a history of melanoma or skin cancer, genetic conditions like xeroderma pigmentosum, systemic lupus erythematosus, and patients unable to adhere to safety protocols.
- Relative Contraindications: Conditions such as photo-induced epilepsy, cataracts, significant liver dysfunction, and age below 16 years require careful consideration.
UVB phototherapy offers several benefits, including its ability to treat localized or full-body conditions, a lower cancer risk compared to PUVA therapy, and the availability of home phototherapy in some cases. It is also a safer and cost-effective alternative to systemic treatments. However, patients must attend frequent appointments, which may be inconvenient for some.
Like any medical treatment, UVB phototherapy has potential risks:
- Short-term Effects: These include dry skin, mild redness, sunburn, or worsening of existing skin conditions. Rarely, it may trigger photodermatoses or reactivation of herpes simplex.
- Long-term Effects:Prolonged treatment may lead to premature skin aging and an increased risk of skin cancer, especially after 500 or more sessions.
Patients undergoing UVB phototherapy should adhere to the following instructions to ensure safety and efficacy:
- Maintain scheduled appointments and allow sufficient time for preparation.
- Inform the doctor about any medical conditions or medications that might increase sensitivity to UV light.
- Avoid applying ointments, cosmetics, or sunscreens unless directed by a healthcare provider. Moisturizers can be applied post-treatment to soothe the skin.
- Protect against additional UV exposure from sunlight or tanning beds.
- Use appropriate protective gear, such as goggles or face masks, during sessions.
- Notify the treatment team promptly about any adverse effects or concerns.
Regular follow-ups with a dermatologist are essential to monitor progress and adjust treatment protocols as needed.
UVB phototherapy remains a cornerstone in the treatment of various dermatological conditions, offering significant improvements in symptoms and quality of life for patients. With proper administration, adherence to safety protocols, and individualized treatment plans, this therapy provides an effective, minimally invasive option for managing chronic skin disorders.



