Steroid rosacea is a skin condition resembling rosacea that develops as a result of prolonged use or withdrawal of potent topical corticosteroids, primarily on the mid-face. It is considered a variant of periorificial dermatitis, a condition that can occur with or without prior steroid use. Unlike steroid acne, which is triggered by oral corticosteroids, steroid rosacea is specifically linked to topical steroid application.
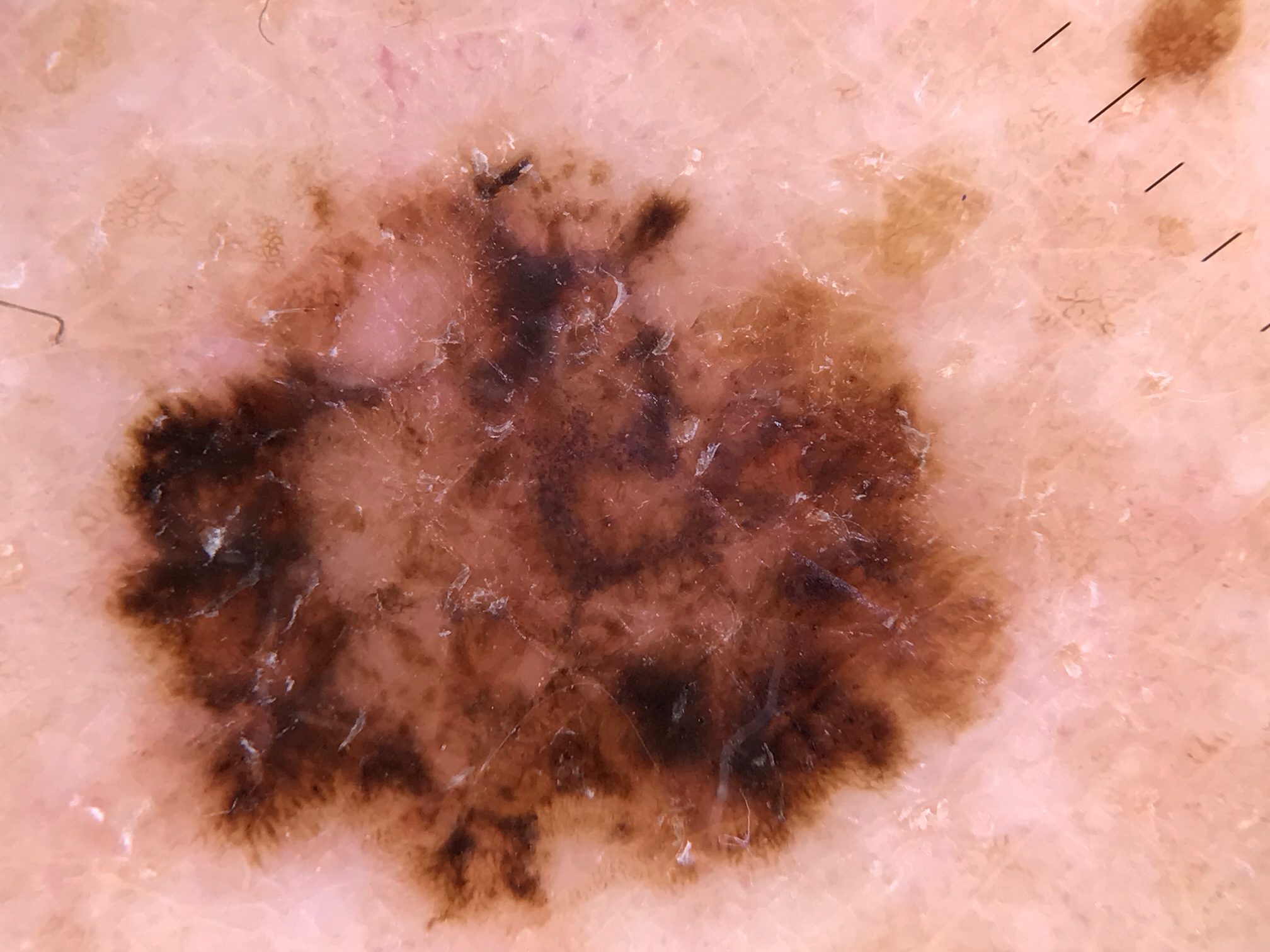
Although steroid rosacea most commonly affects adult women, it can also be seen in men and children. The condition typically emerges after several weeks of applying topical steroids to areas such as the forehead, eyelids, cheeks, or chin. Affected skin becomes red, and small, inflamed bumps or pustules may develop, sometimes accompanied by scaling. The skin often feels excessively warm, irritated, and itchy. Over time, telangiectasia—enlarged and visible blood vessels—may appear, giving the skin a persistent flushed appearance. The affected areas become highly sensitive to skincare products, leading to further discomfort.
One of the most challenging aspects of steroid rosacea is the rebound flare that can occur upon discontinuation of the steroid. This reaction can cause an intense worsening of symptoms, making withdrawal particularly difficult for patients who have relied on steroid treatments for extended periods. The precise mechanism by which topical steroids lead to steroid rosacea is not fully understood, but several theories have been proposed. These include an overgrowth of Demodex mites (tiny organisms that naturally reside in hair follicles), an increase in skin micro-organisms, excessive blood vessel formation leading to rebound vasodilation, and an exaggerated immune response resulting in inflammatory cytokine release.
The severity of steroid rosacea is often linked to the strength and duration of steroid use. Potent steroids applied frequently to facial skin are more likely to trigger the condition, whereas mild steroids used sparingly pose a lower risk. Similar reactions have also been observed following the prolonged use of calcineurin inhibitors, such as tacrolimus ointment and pimecrolimus cream.
Topical steroids can have a range of adverse effects on facial skin, including thinning, increased fragility, and susceptibility to infections. In some cases, steroid rosacea is mistaken for other conditions, such as tinea faciei (a fungal infection of the face) or tinea incognito, a fungal infection that has been masked and altered by prior steroid use. A milder form of steroid-induced rash, known as periorificial dermatitis, presents with small papules around the lips, nose, and eyelids.
The good news is that steroid rosacea usually responds well to treatment, though some lingering telangiectasia may persist. The most effective course of action is to discontinue the use of topical steroids. However, because abrupt withdrawal can lead to a severe flare-up, a gradual reduction in steroid application is recommended. This may involve decreasing the frequency of use and transitioning to a less potent steroid before discontinuing entirely. To support skin recovery, non-oily moisturizers may be used, and in some cases, short-term application of pimecrolimus cream can provide relief.
For more persistent cases, oral tetracycline antibiotics, such as doxycycline, are often prescribed and may be needed for several months to fully control inflammation. If visible blood vessels remain after treatment, vascular laser therapy can be an effective option for reducing telangiectasia and improving the skin’s overall appearance.
While steroid rosacea can be a frustrating condition, understanding its causes and following a carefully managed withdrawal and treatment plan can lead to significant improvement. Consulting a dermatologist for personalized care and guidance is essential for restoring skin health and preventing future flare-ups.