Viral warts represent one of the most common dermatological conditions encountered in clinical practice, manifesting as benign epithelial growths caused by human papillomavirus (HPV) infection. These seemingly simple skin lesions can develop into complex clinical challenges, particularly when they appear in visible areas or prove resistant to standard treatments. While often considered a minor medical concern, warts can cause significant physical discomfort and psychological distress, affecting both quality of life and social interactions. This comprehensive guide explores the intricate nature of viral warts, their transmission mechanisms, diverse clinical presentations, and the array of contemporary treatment approaches available to healthcare providers and patients.
Understanding Viral Warts
Pathophysiology and Transmission
The development of viral warts involves a sophisticated interaction between the human papillomavirus and the host’s epithelial cells. When HPV successfully infiltrates the skin’s basal layer through microscopic breaks or injuries in the epithelium, it initiates a cascade of cellular events that ultimately lead to wart formation. Once inside the cell, the virus triggers several key processes:
- Accelerated cell proliferation, leading to rapid tissue growth
- Altered keratinocyte differentiation, resulting in abnormal skin structure
- Local immune response activation, which varies in effectiveness between individuals
- Formation of characteristic wartlike growths with distinct morphological features
The virus demonstrates remarkable efficiency in transmission through multiple pathways:
- Direct skin-to-skin contact during daily activities
- Autoinoculation from scratching or picking existing lesions
- Indirect contact via contaminated surfaces in shared environments
- Exposure in communal areas like swimming pools and locker rooms
High-Risk Populations
The susceptibility to viral warts varies significantly across different population groups, with certain individuals facing heightened risk due to specific physiological or environmental factors:
- School-Age Children These young individuals face particular vulnerability due to several factors:
- Higher exposure risk through close contact with peers
- Developing immune systems still building viral resistance
- Frequent participation in activities that may cause skin trauma
- Regular exposure in shared recreational spaces
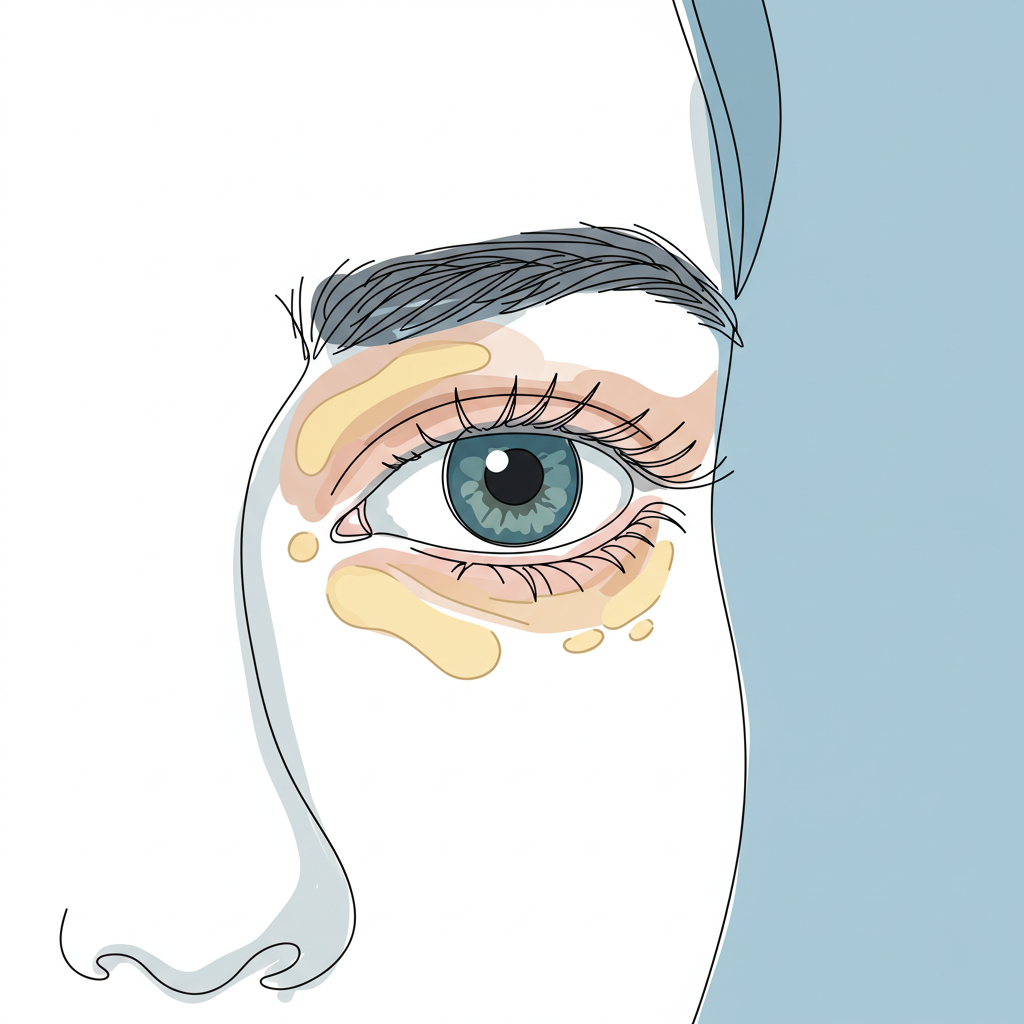
- Individuals with Compromised Skin Barriers Those with underlying skin conditions face additional challenges:
- Eczema patients with disrupted skin integrity
- Individuals with chronic skin conditions affecting barrier function
- People with frequent minor skin injuries from occupational or recreational activities
- Immunocompromised Individuals This group faces particular challenges in both prevention and treatment:
- Patients on immunosuppressive medications following organ transplantation
- HIV-positive individuals with altered immune responses
- Organ transplant recipients requiring ongoing immunosuppression
Clinical Presentation
Physical Characteristics
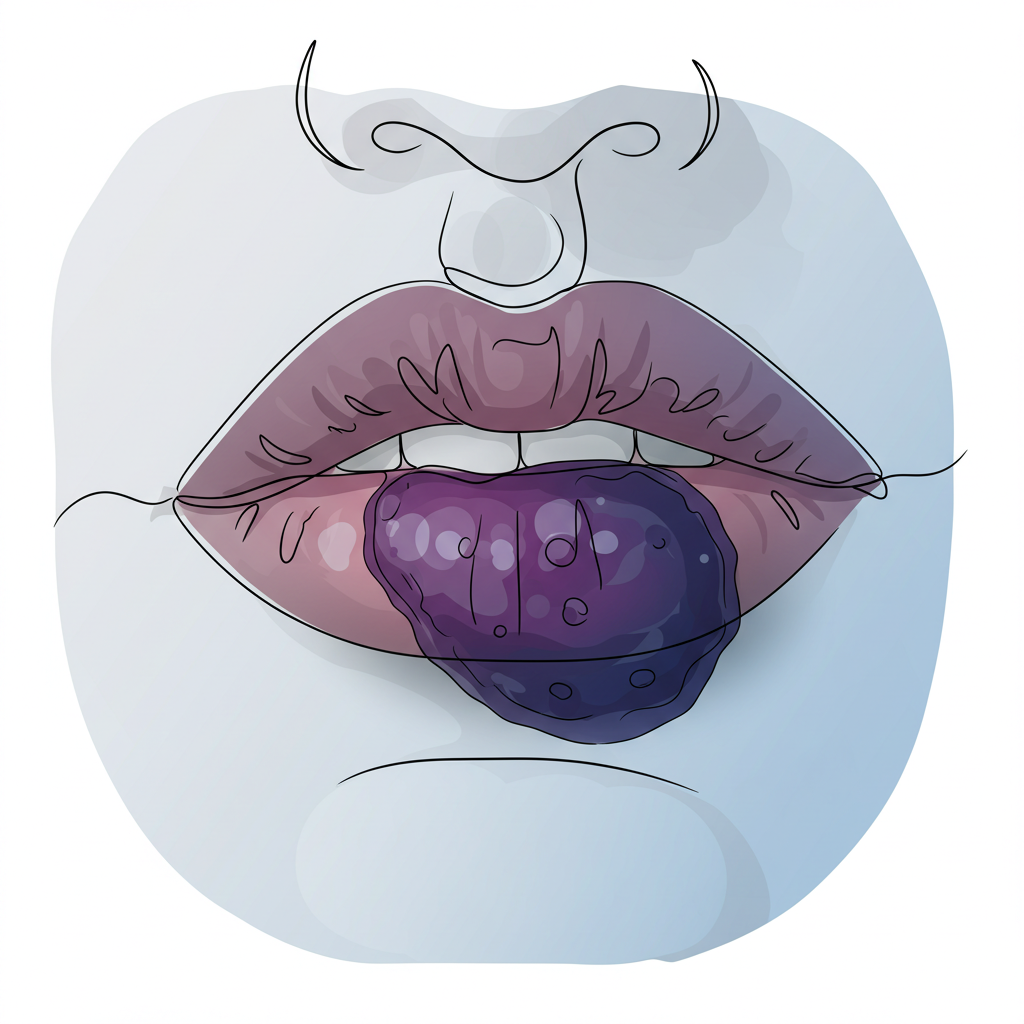
Viral warts exhibit a diverse range of clinical manifestations that can vary significantly based on the specific HPV strain involved and the anatomical location affected. Understanding these distinct features aids both diagnosis and treatment selection. Common presentations include:
- Raised, rough-textured growths that may cluster or appear in isolation
- Keratinous surface texture varying from smooth to deeply fissured
- Variable size and shape, ranging from pinpoint to several centimeters
- Possible presence of black dots (thrombosed capillaries) indicating vascular involvement
- Location-specific morphological variations that reflect local tissue characteristics
The appearance of warts can also be influenced by mechanical factors such as pressure and friction, particularly in weight-bearing areas like the feet. These forces can lead to the development of deeper, more painful lesions that may require more aggressive treatment approaches.
Natural History
The progression and resolution of viral warts follows distinctly different patterns depending on the age of the affected individual and their immune status. Understanding these patterns helps inform treatment decisions and patient counseling:
In Children: The natural course tends to be more favorable, with high rates of spontaneous resolution:
- 50% spontaneous resolution within 6 months, reflecting robust immune responses
- 90% clearance by 2 years without intervention
- Generally better prognosis due to developing immune system adaptation
- More rapid response to therapeutic interventions when needed
In Adults: The clinical course often proves more challenging:
- More persistent presentations requiring longer treatment durations
- Lower rates of spontaneous resolution due to established viral immune evasion
- Often require therapeutic intervention with combination approaches
- Higher risk of recurrence following successful treatment
Treatment Approaches
Conservative Management
The initial approach to wart treatment typically begins with conservative measures, allowing for minimal invasiveness while maintaining therapeutic efficacy:
- Topical Treatments These first-line interventions often prove sufficient for early or uncomplicated cases:
- Salicylic acid preparations in various concentrations
- Over-the-counter wart medications containing keratolytic agents
- Prescription-strength formulations for resistant cases
- Combination therapy with occlusive dressings
- Physical Barrier Methods Essential for both treatment and prevention:
- Occlusive tape application to promote maceration
- Waterproof covering during activities
- Prevention of spread through mechanical barriers
- Regular monitoring and adjustment of barrier techniques
Medical Interventions
When conservative measures prove insufficient, several medical interventions offer enhanced therapeutic potential:
- Cryotherapy This well-established treatment modality utilizes controlled tissue destruction:
- Precise liquid nitrogen application targeting lesional tissue
- Controlled tissue destruction through freeze-thaw cycles
- Multiple sessions often required for complete resolution
- Variable success rates depending on technique and lesion characteristics
- Electrosurgery A more definitive approach for resistant cases:
- Radiofrequency energy application for precise tissue removal
- Local anesthesia requirement for patient comfort
- Higher success rates in resistant cases
- Potential for scarring requiring careful patient selection
- Laser Therapy Advanced treatment option offering targeted intervention:
- Multiple wavelength options for specific lesion types
- Minimal surrounding tissue damage through precise targeting
- Particularly suitable for extensive or resistant warts
- Various treatment protocols available for optimization
Advanced Treatment Options
For patients with resistant or extensive wart infections, modern medicine offers several sophisticated treatment approaches that target different aspects of viral pathogenesis and host immune response:
Immunotherapy This innovative approach harnesses the body’s own immune system to combat viral infections:
- Intralesional immunomodulators stimulating local immune response
- Systemic immune enhancers for widespread involvement
- Custom-tailored protocols based on individual immune status
- Monitoring of immune parameters during treatment
Photodynamic Therapy A specialized intervention combining light activation with photosensitizing agents:
- Selective destruction of virus-infected tissue
- Minimal damage to surrounding healthy cells
- Enhanced cosmetic outcomes in visible areas
- Multiple treatment sessions for optimal results
Combination Treatments Modern therapeutic approaches often integrate multiple modalities to achieve superior outcomes:
- Synchronized application of different treatment methods
- Customized protocols based on lesion characteristics
- Regular assessment of therapeutic response
- Adjustment of treatment intensity as needed
Prevention and Management Strategies
Risk Reduction
Preventing viral wart transmission requires a comprehensive approach to risk management that encompasses both personal and environmental factors:
Personal Hygiene
- Implementation of thorough hand washing protocols
- Regular inspection of skin for early lesion detection
- Proper nail care to prevent traumatic spread
- Use of personal protective equipment when appropriate
Environmental Controls
- Maintenance of clean, dry communal surfaces
- Regular disinfection of shared equipment
- Implementation of proper ventilation systems
- Monitoring of humidity levels in high-risk areas
Ongoing Care
Successful management of viral warts extends beyond initial treatment to encompass long-term monitoring and maintenance:
Regular Assessment
- Scheduled follow-up examinations
- Documentation of treatment response
- Early intervention for new lesions
- Adjustment of management strategies as needed
Preventive Measures
- Strengthening of immune system function
- Optimization of skin barrier health
- Management of underlying medical conditions
- Implementation of lifestyle modifications
Living with Viral Warts
The impact of viral warts often extends far beyond their physical manifestations, affecting multiple aspects of daily life:
Psychological Considerations
- Management of anxiety and self-consciousness
- Development of coping strategies
- Access to support resources
- Building resilience through education
Social Implications
- Navigation of interpersonal relationships
- Participation in recreational activities
- Workplace considerations
- Communication with healthcare providers
Conclusion
Understanding viral warts as a complex dermatological condition requires appreciation of both their biological mechanisms and their impact on patient quality of life. While these lesions often present as benign growths, their management demands a sophisticated approach that addresses both physical and psychosocial aspects of the condition.
The future of wart management continues to evolve with emerging technologies and treatment modalities. Success in treatment often depends on:
- Early recognition and intervention
- Selection of appropriate therapeutic approaches
- Consistent adherence to management protocols
- Regular monitoring and adjustment of treatment strategies
Healthcare providers play a crucial role in guiding patients through the various treatment options and helping them develop effective management strategies. Through comprehensive care and patient education, most individuals can achieve successful outcomes in their journey toward resolution of viral warts.