Rosacea represents a chronic inflammatory skin condition that primarily manifests in the central facial region, affecting millions globally. This intricate disorder extends far beyond simple facial redness, presenting through a complex array of symptoms including persistent erythema, visible blood vessels, and inflammatory lesions that significantly impact both physical appearance and psychological well-being. While the precise etiology remains partially understood, ongoing research continues to illuminate our comprehension of this challenging condition, offering new insights into its management and treatment.
Understanding the Pathophysiology
Rosacea manifests through persistent or recurring episodes of facial inflammation, typically accompanied by sensations of warmth or burning. The condition’s progression often begins with intermittent flushing that gradually intensifies in both frequency and severity over time, creating a cascade of inflammatory responses that can lead to lasting skin changes.
The pathophysiology of rosacea involves a complex interplay of multiple biological systems and environmental factors. Current research identifies several interconnected pathogenic factors that work in concert to produce the characteristic signs and symptoms:
- Genetic Predisposition: Familial patterns suggest strong hereditary components, with specific genetic variations potentially influencing immune response and vascular reactivity
- Environmental Triggers: UV radiation and heat exposure induce vasodilation, leading to prolonged facial flushing and potential vessel damage
- Dietary Influences: Inflammatory responses triggered by specific foods and beverages, particularly those that increase peripheral blood flow
- Microbiological Factors: Demodex folliculorum mite colonization, which may trigger inflammatory cascades and alter skin barrier function
- Immunological Responses: Chronic inflammatory cascade activation, leading to persistent inflammation and tissue damage
- Vascular Dysfunction: Aberrant blood flow patterns and vessel reactivity, contributing to chronic facial erythema and telangiectasia formation
Clinical Manifestations and Subtypes
The presentation of rosacea varies significantly among individuals, with symptoms often evolving over time and potentially overlapping between different subtypes. Understanding these distinct presentations is crucial for appropriate diagnosis and management.
1. Erythematotelangiectatic Rosacea
The classic presentation includes persistent facial redness that represents the foundation of rosacea symptomatology. Key features encompass:
- Persistent facial erythema with trigger-induced exacerbation, often following a characteristic butterfly pattern
- Telangiectatic vessels forming characteristic patterns, particularly visible on the cheeks and nose
- Prolonged flushing episodes that may last hours and cause significant discomfort
- Heightened cutaneous sensitivity, often manifesting as stinging or burning sensations
2. Papulopustular Rosacea
This inflammatory variant presents with distinctive features that often lead to misdiagnosis as acne. However, several key characteristics differentiate this subtype:
- Crops of inflammatory papules and pustules that develop in characteristic patterns
- Acneiform appearance without comedonal lesions, distinguishing it from traditional acne vulgaris
- Preferential central facial distribution, particularly affecting the cheeks, nose, and chin
- Underlying persistent erythema that remains even when inflammatory lesions resolve
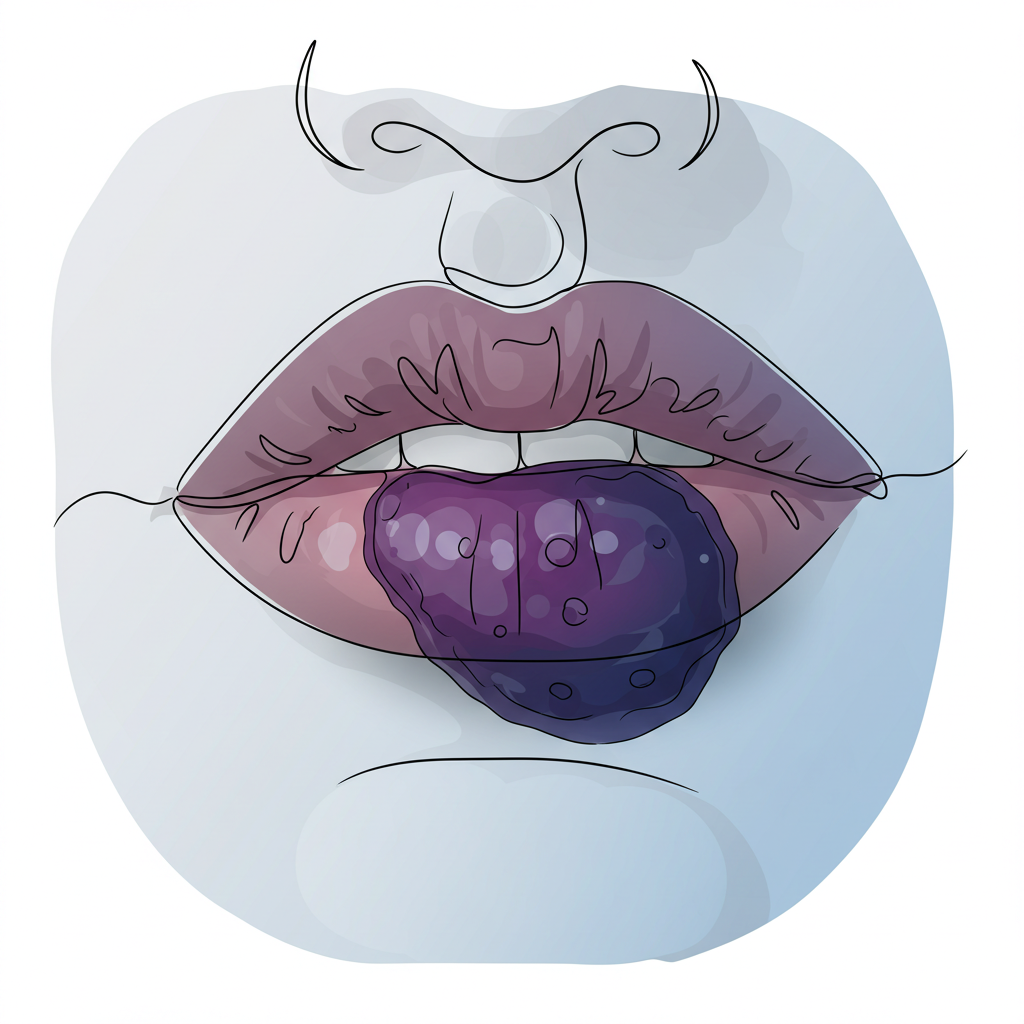
3. Phymatous Rosacea
This advanced form of rosacea involves significant tissue remodeling and represents one of the most challenging variants to treat:
- Progressive fibrotic changes and surface irregularity developing over months to years
- Predominant rhinophyma development, characterized by nasal enlargement and tissue thickening
- Potential involvement of additional facial sites, including the chin, forehead, and ears
- Male predominance suggesting hormonal influence in disease progression
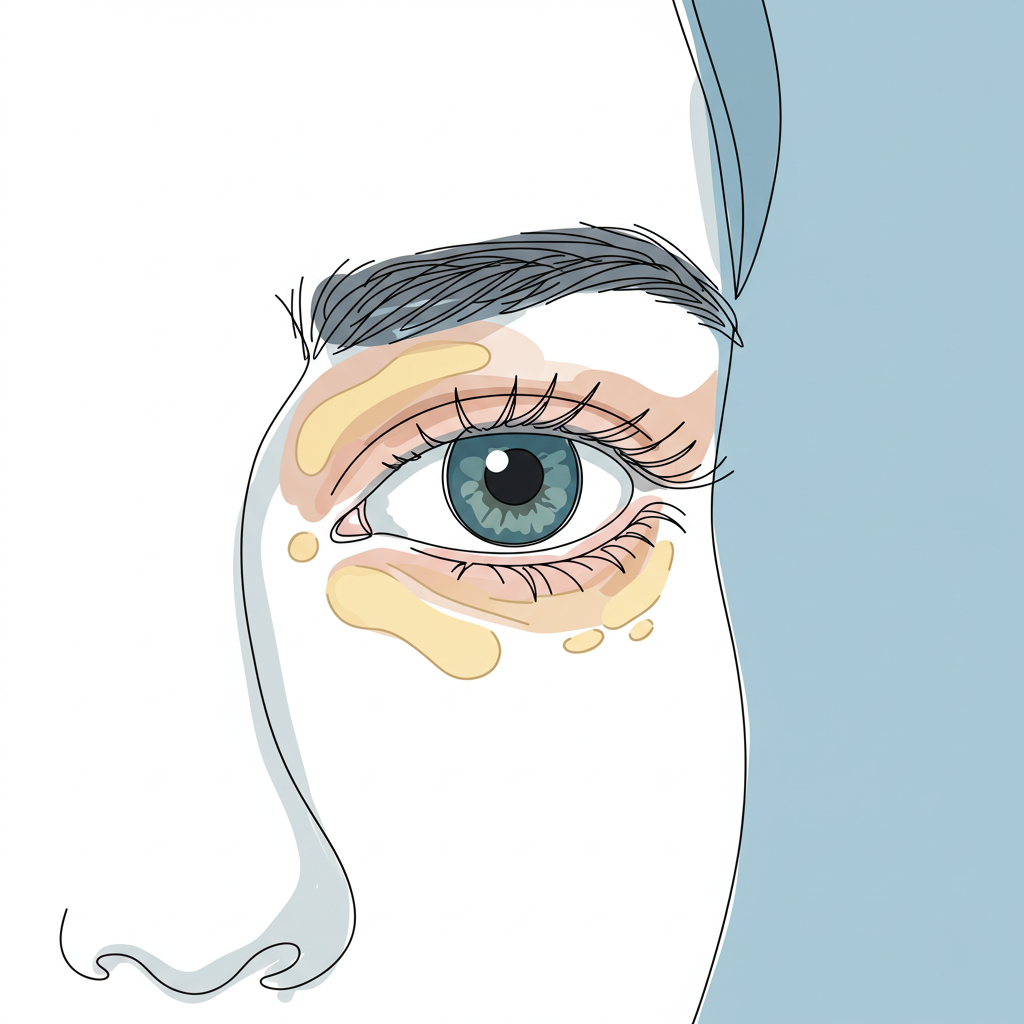
4. Ocular Rosacea
Ocular involvement represents a potentially serious manifestation requiring specialized attention:
- Concurrent or preceding ocular inflammation that may develop before cutaneous symptoms
- Chronic blepharitis leading to persistent eye discomfort and visual disturbance
- Significant dry eye symptomatology affecting daily activities and quality of life
- Risk of vision-threatening complications if left untreated
Therapeutic Approach
The management of rosacea requires a sophisticated, multi-modal approach that addresses both immediate symptoms and long-term disease control. Success often depends on combining various therapeutic strategies while maintaining consistent adherence to preventive measures.
Preventative Strategies
The foundation of rosacea management relies on careful trigger identification and systematic avoidance protocols. Understanding and implementing these preventative measures can significantly reduce the frequency and severity of flare-ups.
- Solar Protection The cornerstone of prevention centers on comprehensive photoprotection:
- Implementation of broad-spectrum photoprotection using SPF 30 or higher daily
- Selection of sensitive skin-specific formulations that avoid common irritants
- Regular reapplication, particularly during extended sun exposure
- Use of physical barriers such as wide-brimmed hats and UV-protective clothing
- Environmental Modifications Creating a skin-friendly environment plays a crucial role in management:
- Temperature regulation through careful climate control
- Humidity control to maintain optimal skin barrier function
- Avoidance of extreme weather exposure, including both hot and cold conditions
- Implementation of protective measures during challenging weather conditions
- Dietary Management A systematic approach to dietary triggers can significantly impact disease control:
- Identification of individual triggers through detailed food and symptom logging
- Implementation of structured elimination protocols under medical supervision
- Careful reintroduction testing to confirm specific trigger foods
- Development of a sustainable, balanced diet that avoids known triggers
Medical Interventions
The medical management of rosacea typically follows a stepwise approach, beginning with topical treatments and progressing to systemic therapy as needed. Success often requires careful monitoring and adjustment of therapeutic strategies.
Topical Therapeutics
First-line interventions form the backbone of treatment for many patients:
- Metronidazole preparations, available in various strengths and formulations
- Azelaic acid formulations that target both inflammation and redness
- Ivermectin-based treatments, particularly effective for demodex-associated symptoms
- Selected calcineurin inhibitors for steroid-sparing anti-inflammatory effects
These topical agents work through multiple mechanisms to reduce inflammation, control microbial factors, and improve skin barrier function. Regular application and proper technique are essential for optimal results.
Systemic Therapy
For moderate to severe presentations, systemic treatments may become necessary:
- Anti-inflammatory dose doxycycline, specifically formulated to avoid antimicrobial effects
- Low-dose isotretinoin protocols carefully monitored for side effects
- Strict avoidance of corticosteroids to prevent rebound flares
- Regular monitoring of treatment response and potential side effects
Advanced Treatment Modalities
For patients with persistent symptoms or specific concerns, advanced interventions can provide significant benefit:
Energy-based interventions utilize cutting-edge technology to target specific aspects of rosacea:
- IPL therapy for vascular component reduction and overall redness improvement
- Targeted laser treatments for precise telangiectasia elimination
- Contemporary light-based technologies offering customized treatment approaches
These advanced treatments often require multiple sessions for optimal results and may need periodic maintenance treatments to sustain improvements.
Living with Rosacea
Living with rosacea extends beyond medical management to encompass lifestyle modifications and psychological adaptation. While rosacea represents a chronic condition without definitive cure, implementing comprehensive management strategies significantly improves outcomes. Success depends on developing individualized approaches addressing specific triggers and manifestations.
The psychological impact of rosacea should not be underestimated, as the visible nature of the condition can significantly affect self-esteem and social interactions. Support groups and counseling may provide valuable additional resources for coping with these challenges.
Conclusion
Effective rosacea management requires a sophisticated understanding of its chronic nature combined with committed long-term care strategies. Through appropriate medical intervention, consistent preventive measures, and lifestyle modification, most patients achieve substantial symptomatic improvement and enhanced quality of life.
The future of rosacea treatment continues to evolve, with ongoing research into new therapeutic targets and treatment modalities offering hope for even more effective management strategies. Regular follow-up with healthcare providers ensures that treatment plans remain optimized for individual patient needs and respond to changing disease patterns.