Psoriasis represents one of the most common chronic inflammatory skin conditions affecting millions worldwide, impacting not just the skin but also patients’ emotional wellbeing and daily lives. This comprehensive overview explores the intricate nature of psoriasis, diving deep into its underlying causes, diverse symptom presentations, and the sophisticated treatment approaches available in modern dermatology.
What is Psoriasis?
Psoriasis is a persistent autoimmune condition that affects the skin, causing cells to build up rapidly on the surface. This accelerated cell turnover, occurring much faster than in healthy skin, results in thick, distinctive plaques characterized by well-defined red patches covered with silvery-white scales. The buildup occurs because the body’s immune system mistakenly signals skin cells to grow at an abnormally rapid pace, creating a cycle of inflammation that manifests as visible skin changes. While often considered merely a skin condition, psoriasis actually reflects a complex internal inflammatory process that can impact multiple body systems, potentially affecting joints, cardiovascular health, and metabolic function.
Epidemiology and Demographics
The condition affects approximately 2-4% of the North American population, showing no preference between males and females. This prevalence translates to millions of individuals living with varying degrees of psoriasis severity, each experiencing unique challenges in managing their condition. Psoriasis exhibits an interesting bimodal age distribution, with two distinct peak onset periods:
- Early-onset (Type 1): Typically occurs between 15-25 years of age, often presenting with more severe symptoms and stronger genetic associations
- Late-onset (Type 2): Generally develops between 50-60 years of age, frequently showing milder manifestations but potentially complicated by other age-related health conditions
Understanding the Causes
Psoriasis emerges from a complex interplay of genetic and environmental factors, representing a fascinating example of how genetics and environment interact to influence disease development. The genetic component plays a particularly significant role, with approximately one-third of patients reporting a family history of the condition, suggesting a strong hereditary influence. Several triggering factors can initiate or exacerbate psoriasis flares:
- Psychological stress, which can activate inflammatory pathways in the body
- Excessive alcohol consumption, potentially disrupting immune system function
- Obesity and metabolic disorders, contributing to systemic inflammation
- Physical trauma to the skin (known as the Koebner phenomenon), where skin injury triggers psoriatic lesions
- Sudden discontinuation of oral corticosteroids, causing rebound inflammation
- Certain medications that may interfere with immune system regulation
- Infections, particularly streptococcal infections, which can trigger initial onset or flares
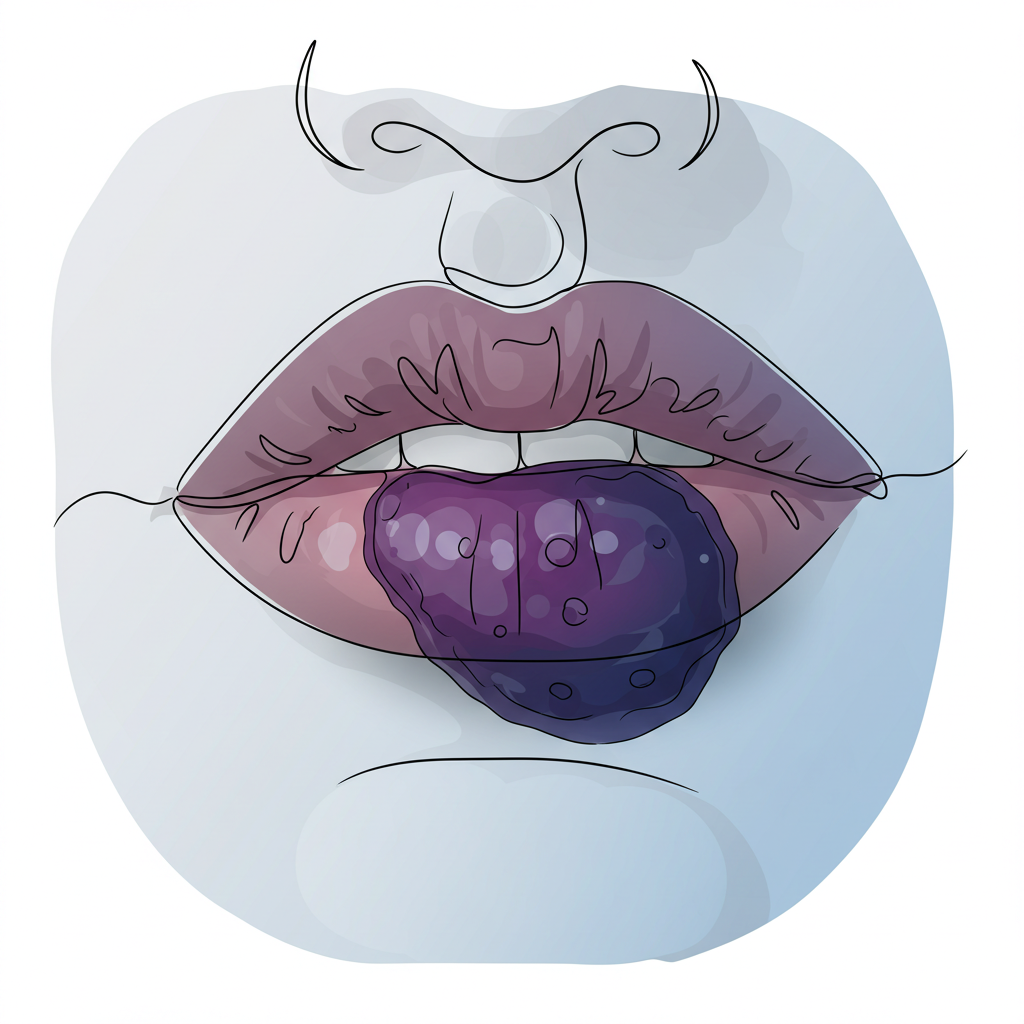
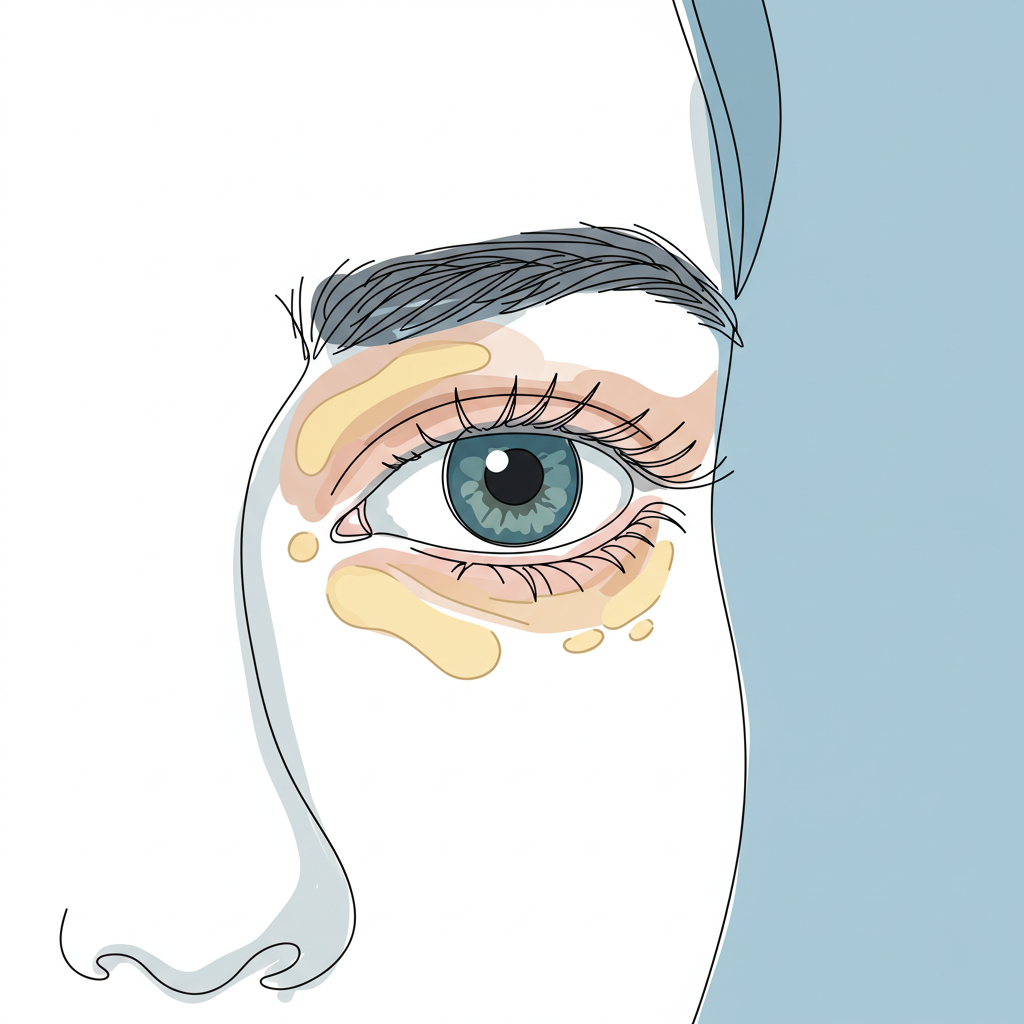
Clinical Presentation and Distribution
The hallmark of psoriasis is its distinctive appearance and distribution pattern, which often follows a symmetrical arrangement that helps differentiate it from other skin conditions. Lesions typically present as:
- Symmetrically distributed plaques on both sides of the body, reflecting the systemic nature of the condition
- Well-demarcated, raised red patches that feel warm to the touch
- Silvery-white scale covering the red patches, often thick and adherent
- Variable size, from small spots to large patches that may merge into larger affected areas
While psoriasis can affect any area of the skin, certain locations are particularly common, often following a pattern that reflects areas of frequent friction or pressure:
- Elbows and knees (especially the extensor surfaces), where mechanical stress is common
- Scalp, which can be particularly challenging to treat due to hair coverage
- Lower back, often affecting the sacral region
- Nail beds, causing characteristic pitting and discoloration
- Palms and soles, which can significantly impact daily activities
- Skin folds (in certain variants), presenting unique treatment challenges
Treatment Approaches
Modern psoriasis management employs a sophisticated, stepped approach, carefully tailoring treatments to disease severity, patient factors, and individual response patterns. This personalized strategy recognizes that psoriasis manifests differently in each person and that treatment success often requires a combination of approaches. Current therapeutic options include:
Topical Therapy
The first-line treatment for mild to moderate psoriasis encompasses a range of carefully formulated medications applied directly to affected areas. These include:
- Corticosteroids of varying potencies, which target inflammation and cell proliferation
- Vitamin D analogs that help normalize skin cell growth patterns
- Tar-based preparations that have both anti-inflammatory and anti-scaling properties
- Topical retinoids that modulate cell differentiation and reduce inflammation
- Calcineurin inhibitors, particularly useful for sensitive areas and facial involvement
Each of these options can be used alone or in strategic combinations to maximize therapeutic benefit while minimizing side effects.
Phototherapy
Controlled exposure to ultraviolet radiation (UVB or PUVA) represents a time-tested treatment modality that can effectively reduce inflammation and slow cell turnover. This therapeutic approach harnesses the power of specific wavelengths of light to:
- Modulate immune system response in the skin
- Reduce inflammatory cell activity
- Normalize keratinocyte proliferation rates
- Improve skin barrier function
Treatment protocols are carefully calibrated to each patient’s skin type and disease severity, with sessions typically scheduled several times per week for optimal results.
Systemic Treatments
For moderate to severe cases, immunosuppressive medications offer powerful disease control options. These medications work throughout the body to modulate immune response and reduce inflammation. Common options include:
- Methotrexate, which affects DNA synthesis and immune cell function
- Cyclosporine, targeting specific immune pathways
- Oral retinoids, which help normalize skin cell development
- Apremilast, a newer option that modulates inflammatory signaling
These treatments require careful monitoring and regular blood tests to ensure safety and optimize effectiveness.
Biologics
The newest class of treatments represents a revolutionary approach to psoriasis management, targeting specific components of the immune system involved in psoriasis development. These sophisticated medications have transformed the treatment landscape for severe cases by:
- Precisely targeting key inflammatory molecules
- Providing long-lasting disease control
- Offering improved safety profiles compared to traditional systemics
- Potentially preventing disease progression and comorbidity development
Living with Psoriasis
Managing psoriasis extends well beyond medical treatment, requiring a holistic approach that addresses both physical and psychological aspects of the condition. Lifestyle modifications and self-care strategies play crucial roles in disease management:
- Maintaining a healthy weight through balanced nutrition and portion control
- Regular exercise, which reduces inflammation and improves overall health
- Stress management techniques, including mindfulness, meditation, and relaxation practices
- Proper skin care and moisturizing routines tailored to individual needs
- Avoiding known triggers through careful monitoring and lifestyle adjustments
- Building a strong support network of healthcare providers, family, and fellow patients
These comprehensive lifestyle approaches complement medical treatments and help maintain long-term disease control.
Conclusion
While psoriasis presents significant challenges, modern treatment options and comprehensive management strategies offer hope for effective control. The condition’s complex nature requires a nuanced understanding of both its physical manifestations and psychological impact. By approaching treatment through multiple complementary strategies, many patients can achieve significant improvement in their symptoms and quality of life.
Research continues to advance our understanding of psoriasis and develop increasingly effective treatments. This progress, combined with holistic management approaches, provides growing optimism for the psoriasis community. Understanding the condition’s nature and available treatments empowers patients to work collaboratively with healthcare providers in developing optimal management plans.
Remember to consult with healthcare professionals for personalized advice and treatment options, as psoriasis management should be tailored to individual needs and circumstances. Regular follow-up care, open communication with healthcare providers, and consistent adherence to treatment plans provide the best foundation for long-term success in managing this chronic condition.