Melasma represents one of dermatology’s most intricate and psychologically impactful pigmentary disorders, affecting millions of individuals worldwide who struggle daily with its visible manifestations. This comprehensive guide delves deep into the complexities of melasma, exploring everything from its subtle underlying causes to the latest advances in treatment approaches, offering hope and understanding to both patients and healthcare providers navigating this challenging condition.
What is Melasma?
Melasma manifests as a chronic skin condition characterized by symmetrical, blotchy, and brownish facial pigmentation that develops gradually over time, often catching individuals unaware as it slowly progresses. This complex disorder disrupts the normal functioning of the skin’s melanin-producing cells, resulting in distinctive patches of discoloration that can profoundly impact an individual’s appearance, self-perception, and social interactions. Unlike many other pigmentary disorders, melasma’s persistent nature and tendency to worsen with sun exposure make it particularly challenging to manage effectively.
Epidemiology and Risk Factors
The distribution of melasma across diverse populations reveals fascinating patterns that illuminate its underlying mechanisms and help healthcare providers better understand its selective impact:
Demographic Patterns
Through extensive clinical observation and research, clear patterns have emerged regarding who is most likely to develop melasma:
- Predominantly affects women (75% of cases), suggesting a strong hormonal component
- Typically emerges between ages 20-40, coinciding with peak reproductive years
- Higher prevalence in individuals with naturally brown skin, indicating melanin sensitivity
- Less common in extremely fair or dark skin types, though no ethnicity is completely immune
Risk Assessment
Individual susceptibility to melasma varies significantly based on several key characteristics:
- Fitzpatrick skin types III-V (those who tan well) show increased vulnerability
- Female gender, particularly during reproductive years, due to hormonal influences
- Genetic predisposition plays a crucial role in determining susceptibility
- History of sun exposure acts as a primary trigger and exacerbating factor
- Hormonal fluctuations create windows of increased vulnerability
Understanding the Causes
Melasma’s development involves a complex interplay of multiple triggering factors, creating a challenging condition that requires careful understanding for effective management. The intricate relationship between these various factors helps explain why melasma can be so resistant to treatment and prone to recurrence.
Primary Triggers
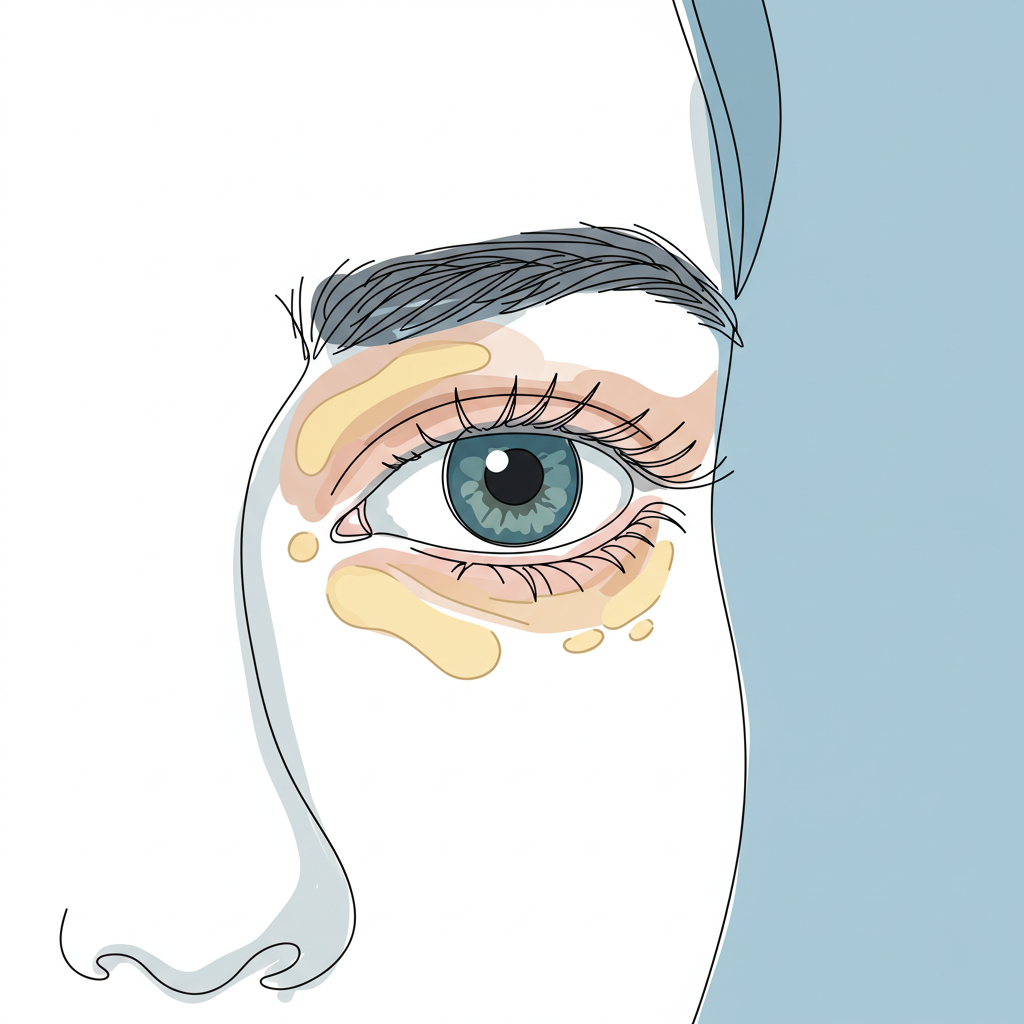
- Sun Exposure and Photodamage The relationship between melasma and ultraviolet radiation represents one of the most crucial aspects of the condition’s development and progression:
- UV radiation actively stimulates melanin production, triggering immediate pigmentary responses
- Visible light, especially blue light from electronic devices and LED lighting, can worsen pigmentation in susceptible individuals
- Cumulative damage contributes to condition persistence, creating a cycle of pigmentation that becomes increasingly difficult to break
- Hormonal Influences The strong connection between hormonal fluctuations and melasma development helps explain its prevalence in certain populations:
- Pregnancy often triggers the condition (known as chloasma or “mask of pregnancy”), affecting up to 70% of pregnant women
- Oral contraceptive use can initiate or exacerbate existing melasma patches
- Hormone replacement therapy may trigger pigmentary changes in susceptible individuals
- Thyroid dysfunction, particularly hypothyroidism, creates an internal environment conducive to melasma development
- External Factors Environmental and lifestyle factors play a significant role in both the development and maintenance of melasma:
- Certain cosmetic products can irritate the skin and trigger pigmentation
- Scented or deodorant soaps may contain photosensitizing ingredients
- Photosensitizing medications increase susceptibility to UV-induced pigmentation
- Heat exposure and inflammation can stimulate melanin production
Clinical Presentation
Melasma presents with distinctive characteristics that set it apart from other pigmentary disorders, making accurate diagnosis possible through careful clinical observation. Understanding these patterns helps both healthcare providers and patients recognize the condition early and initiate appropriate treatment.
Key Features
The hallmark signs of melasma create a recognizable pattern that often displays:
- Symmetrical distribution on both sides of the face, creating a mirror-like appearance
- Brown to gray-brown patches that can vary in intensity
- Irregular but well-defined borders that create map-like patterns
- Common locations include several characteristic facial zones:
- Cheeks, often the most prominently affected area
- Forehead, typically in a symmetrical pattern
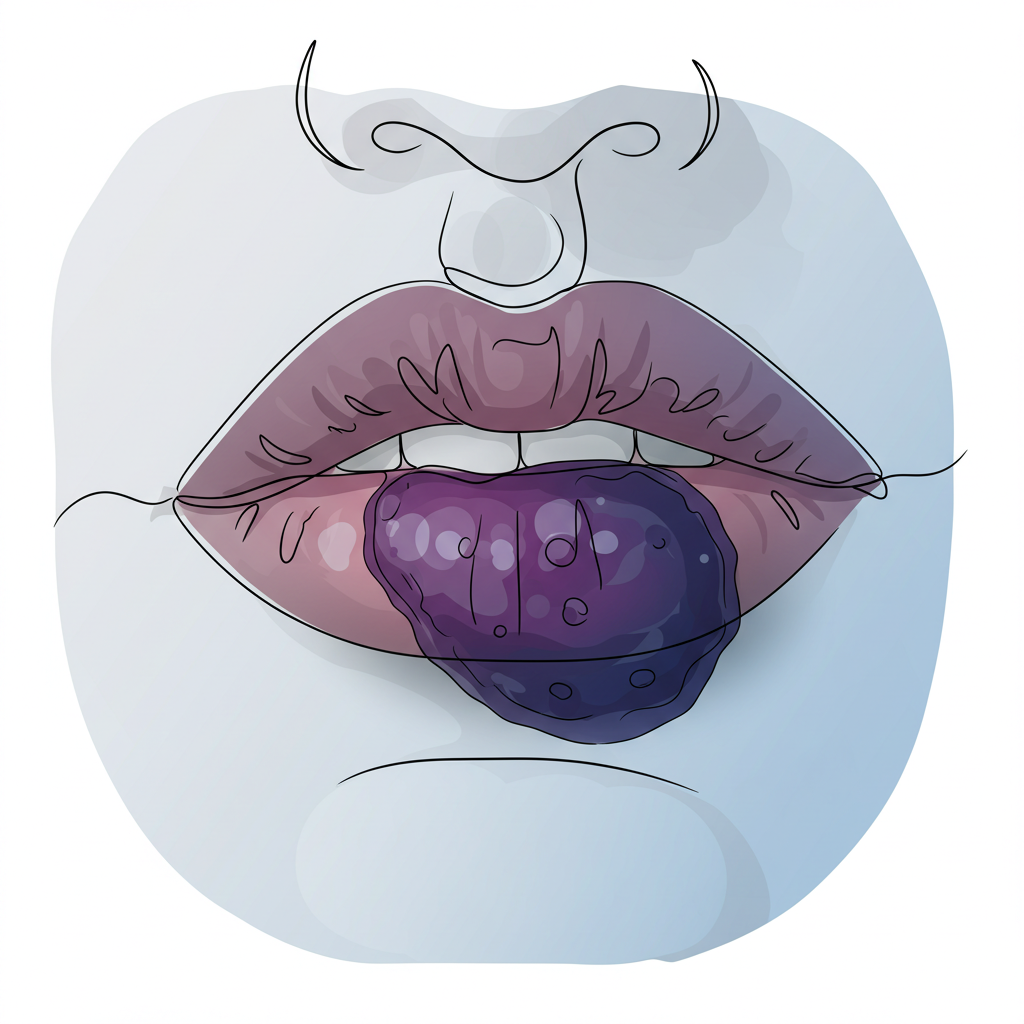
- Upper lip, creating a distinctive mustache-like appearance
- Bridge of nose, connecting other affected areas
- Chin, frequently showing bilateral involvement
Pattern Types
Melasma manifests in three primary distribution patterns, each with its own characteristics and treatment considerations:
- Centrofacial Pattern This most common presentation creates a characteristic mask-like appearance:
- Affects forehead, cheeks, nose, upper lip, and chin
- Creates a butterfly-like distribution across the central face
- Often the most psychologically impacting pattern due to its visibility
- Malar Pattern A more limited but still significant presentation:
- Primarily appears on cheeks and nose
- Creates a distinctive flush-like appearance
- May be mistaken for other conditions like rosacea
- Mandibular Pattern The least common but often most resistant pattern:
- Occurs along the jawline
- Frequently associated with hormonal influences
- Can be particularly challenging to treat
Treatment Approaches
Managing melasma requires a sophisticated, patient-tailored approach that acknowledges both its chronic nature and the significant impact it has on patients’ quality of life. Success often depends on combining multiple therapeutic modalities while maintaining vigilant preventive measures.
Topical Therapies
First-line treatments form the foundation of most melasma management protocols, targeting the condition through various mechanisms of action:
- Hydroquinone 2–4% This gold-standard treatment operates through specific biological pathways:
- Available in carefully formulated cream or lotion forms
- Inhibits tyrosinase enzyme activity, directly affecting melanin production
- Requires careful monitoring for side effects, including potential paradoxical darkening
- Treatment duration must be carefully managed to prevent complications
- Vitamin C (Ascorbic Acid) This powerful antioxidant offers multiple benefits for melasma patients:
- Provides potent antioxidant properties that protect against UV damage
- Helps reduce melanin production through natural pathways
- Supports skin barrier function, improving overall skin health
- Can be combined safely with other treatments for enhanced results
- Methimazole This emerging treatment option shows promising results:
- Novel treatment mechanism differs from traditional approaches
- Shows particular promise in cases resistant to conventional therapy
- Offers potential for long-term management
- Requires careful monitoring and professional oversight
- Azelaic Acid A versatile treatment option with multiple beneficial effects:
- Available in various formulations for personalized treatment
- Well-tolerated by most patients, making it suitable for long-term use
- Provides dual anti-inflammatory and lightening effects
- Can be integrated effectively into combination protocols
Advanced Treatment Options
Modern dermatology offers sophisticated interventions for resistant cases:
Device-Based Treatments
These technological approaches provide targeted therapy:
- Laser therapy utilizing specific wavelengths for precise pigmentation targeting
- Intense Pulsed Light (IPL) treatments offering broad-spectrum improvement
- Chemical peels of varying depths for controlled exfoliation
- Microneedling to enhance product penetration and stimulate collagen
Combination Approaches
Success often lies in carefully orchestrated treatment combinations:
- Comprehensive sun protection strategies integrated with active treatments
- Synergistic topical agent combinations
- Strategic timing of procedural interventions
- Carefully planned maintenance protocols to prevent recurrence
Prevention and Management
The cornerstone of successful melasma management lies in prevention and consistent maintenance. This requires a comprehensive approach that addresses multiple aspects of skin health and protection.
Essential Prevention Steps
- Sun Protection Vigilant sun protection forms the foundation of melasma management:
- Daily application of broad-spectrum sunscreen (SPF 30+) with frequent reapplication
- Implementation of physical sun protection measures through protective clothing
- Strategic avoidance of peak UV hours to minimize exposure
- Understanding and protecting against visible light exposure
- Trigger Avoidance Careful monitoring and elimination of known triggers:
- Methodical selection of skincare products to avoid irritation
- Regular assessment of hormonal medications and their effects
- Implementation of strategies to prevent heat-induced inflammation
- Awareness of environmental factors that may exacerbate the condition
- Regular Monitoring Professional oversight ensures optimal management:
- Scheduled professional skin assessments to track progress
- Systematic photography documentation to measure changes
- Dynamic treatment adjustment based on response and seasonal variations
- Regular review and updating of management strategies
Living with Melasma
Successfully managing melasma extends beyond medical treatment to encompass lifestyle adaptations and psychological support. Patients must develop a comprehensive understanding of their condition while maintaining realistic expectations about treatment outcomes. This involves:
- Accepting the chronic nature of the condition while remaining optimistic about management options
- Maintaining unwavering commitment to long-term prevention strategies
- Developing strong emotional support networks and coping mechanisms
- Establishing regular dermatological care relationships for ongoing monitoring
Conclusion
Melasma represents one of dermatology’s most complex and challenging conditions, requiring a thorough understanding of its multifaceted nature for effective management. While a complete cure remains elusive, modern treatment approaches offer unprecedented hope for significant improvement. Success lies in combining appropriate medical interventions with rigorous prevention strategies and comprehensive patient education.
The journey to managing melasma demands patience, persistence, and a strong partnership between healthcare providers and patients. Through careful adherence to treatment protocols and preventive measures, many individuals can achieve meaningful improvement in their condition, leading to enhanced confidence and quality of life. Remember that each case is unique, requiring individualized attention and ongoing adjustment of treatment strategies for optimal results.