In dermatology, few conditions demand as much attention and careful management as Actinic Keratosis (AK). This comprehensive guide explores the intricacies of this common pre-cancerous skin condition, offering valuable insights into its recognition, treatment, and prevention. As our understanding of skin health continues to evolve, the importance of early intervention in managing AK has become increasingly apparent.
Understanding Actinic Keratosis: A Precursor to Skin Cancer
Actinic Keratosis develops when skin cells sustain cumulative damage from ultraviolet (UV) radiation exposure, primarily from sunlight. These lesions serve as crucial warning signs, indicating significant sun damage that requires medical attention. Like silent sentinels on the skin’s surface, AK lesions alert both patients and healthcare providers to potential underlying damage that extends beyond visible changes. Understanding their nature and progression is essential for both healthcare providers and patients in managing this condition effectively.
The transformation from healthy skin cells to precancerous lesions occurs gradually, often over decades of sun exposure. This slow progression makes early recognition particularly crucial, as intervention during early stages can prevent further development into more serious conditions.
Risk Factors and Contributing Elements
The development of Actinic Keratosis involves a complex interplay of genetic, environmental, and lifestyle factors. Understanding these risk elements helps healthcare providers develop targeted prevention strategies and enables patients to make informed decisions about their sun protection habits.
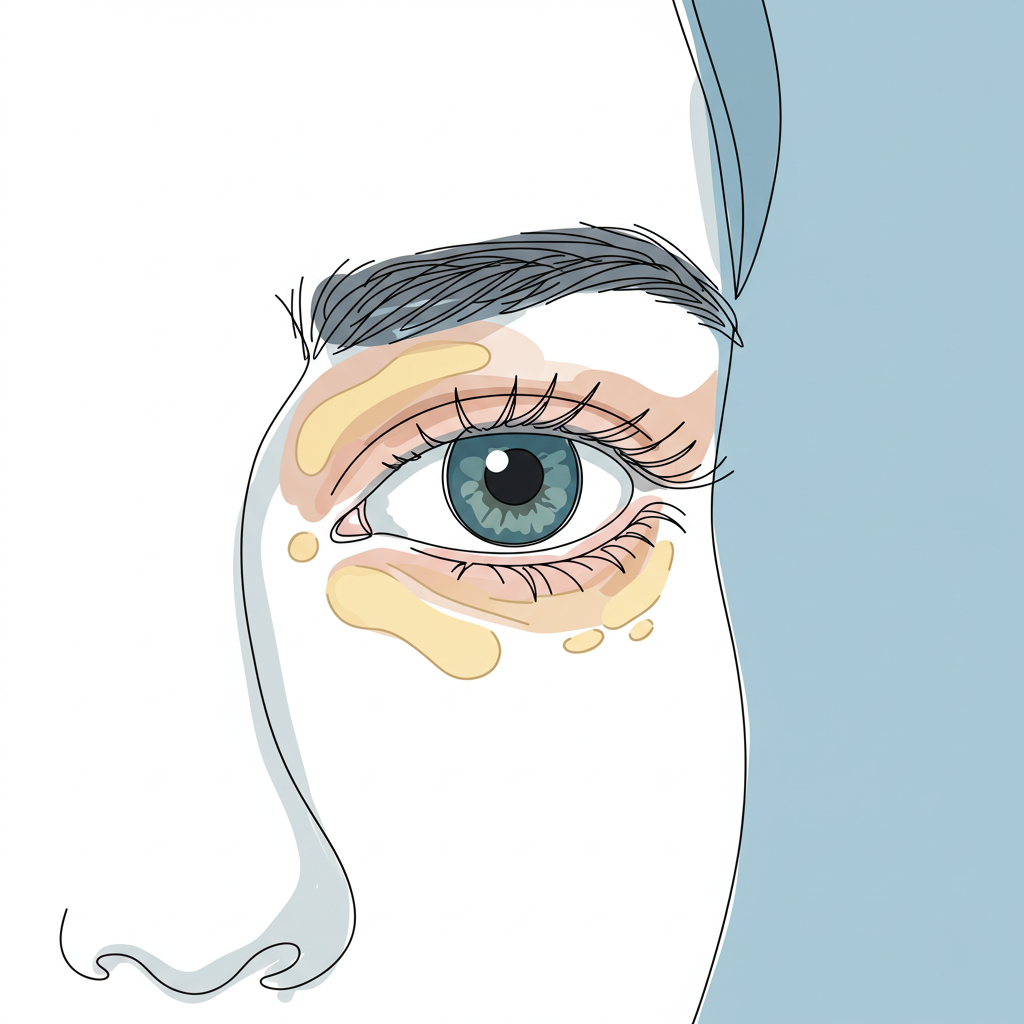
- Genetic Predisposition: Individuals with fair skin, light-colored hair, and blue or green eyes face significantly higher risks of developing AK lesions due to reduced natural UV protection. Their skin contains less melanin, the pigment that provides natural defense against UV radiation.
- Cumulative Sun Exposure: Years of unprotected sun exposure create a compounding effect, making adults over 40 particularly susceptible to developing these lesions. Each instance of sun exposure adds to the cumulative damage, much like pages adding to a book of skin history.
- Environmental and Lifestyle Factors: Regular outdoor activities, residence in sunny climates, and use of tanning beds can accelerate the development of AK lesions. Professional outdoor workers, such as farmers and construction workers, face particularly high risks due to their sustained sun exposure.
- Medical Considerations: Compromised immune systems and certain photosensitizing medications can increase susceptibility to UV damage and subsequent AK formation. This vulnerability highlights the importance of comprehensive medical history evaluation in risk assessment.
Clinical Presentation and Identification
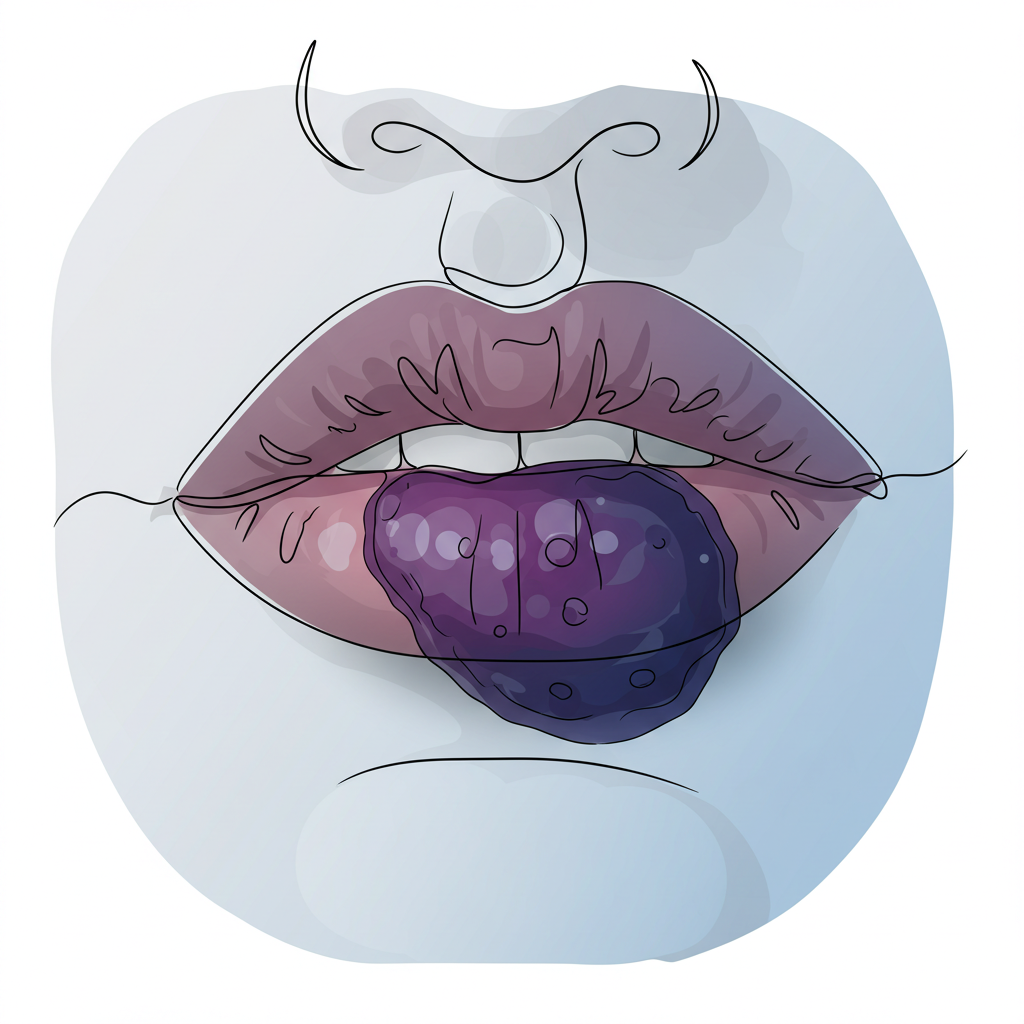
Actinic Keratosis presents with remarkable variability, making familiarity with its various manifestations crucial for early detection. The lesions often appear subtly at first, gradually becoming more pronounced over time.
- Physical Appearance: Lesions typically present as rough, scaly patches with a sandpaper-like texture, ranging in color from pink to red or matching the surrounding skin tone. These patches may be easier to feel than see initially, emphasizing the importance of both visual and tactile examination.
- Distribution Pattern: These lesions show a marked preference for sun-exposed areas, particularly affecting the face, forehead, bald scalp, neck, hands, and upper chest. This pattern reflects the cumulative impact of sun exposure on vulnerable skin surfaces.
- Progressive Changes: Some lesions may remain flat while others become elevated, with potential variations in pigmentation and occasional symptoms of irritation or itching. This dynamic nature of AK lesions necessitates ongoing monitoring and assessment.
Medical Implications and Diagnostic Process
The significance of Actinic Keratosis extends far beyond its immediate presentation, primarily due to its potential progression to squamous cell carcinoma (SCC). When multiple lesions are present, the cumulative risk of malignant transformation increases substantially, creating a complex medical scenario that demands thorough evaluation and consistent monitoring.
The relationship between AK and skin cancer represents a critical continuum in dermatological oncology. Studies suggest that approximately 5-10% of AK lesions may progress to SCC if left untreated, highlighting the importance of early intervention. This progression risk becomes particularly significant in patients with extensive sun damage or compromised immune function.
Dermatologists employ a sophisticated diagnostic approach that combines several complementary methods:
- Visual Examination: Careful assessment of lesion characteristics and distribution patterns forms the cornerstone of diagnosis. Dermatologists evaluate subtle variations in color, texture, and border definition that might indicate progression or transformation.
- Physical Assessment: Evaluation of texture and associated symptoms provides crucial tactile information. The characteristic sandpaper-like feel of AK lesions often serves as a key diagnostic indicator, complementing visual findings.
- Selective Biopsy: Additional testing for suspicious lesions or those resistant to treatment may be necessary. This process involves microscopic examination of tissue samples to determine the exact nature and extent of cellular changes.
Contemporary Treatment Approaches
Modern dermatology has evolved to offer an impressive array of treatment modalities, each tailored to address specific presentations of Actinic Keratosis. The selection of appropriate treatment strategies depends on factors including lesion characteristics, patient preferences, and overall health status.
- Targeted Therapies:
- Cryotherapy with liquid nitrogen remains the gold standard for individual lesions, offering precise destruction of abnormal tissue while preserving surrounding healthy skin
- Surgical removal through shave excision or curettage provides definitive treatment for thicker or suspicious lesions
- Electrodesiccation for persistent cases offers an alternative approach when other methods prove insufficient
- Field Therapy Options:
- Topical medications including diclofenac gel and 5-Fluorouracil cream address both visible lesions and subclinical damage
- Imiquimod cream stimulates local immune response modification, helping the body recognize and eliminate abnormal cells
- Ingenol mebutate gel provides targeted treatment with a shorter duration of application
- Photodynamic therapy combines photosensitizing agents with controlled light exposure for comprehensive field treatment
The approach to treating multiple lesions often requires a combination of therapies, strategically selected to maximize efficacy while minimizing side effects. This integrated treatment paradigm reflects our growing understanding of AK as both a local and field condition requiring comprehensive management.
Prevention and Long-Term Care Strategies
The cornerstone of Actinic Keratosis management lies in prevention and ongoing surveillance. A comprehensive preventive strategy incorporates both protective measures and behavioral modifications, creating a robust defense against further UV damage.
- Daily Sun Protection:
- Use of broad-spectrum SPF 30+ sunscreen forms the foundation of prevention
- Regular reapplication, especially during extended outdoor exposure, ensures continuous protection
- Protective clothing including wide-brimmed hats and UV-blocking fabrics provides additional defense against harmful radiation
- Behavioral Modifications:
- Avoiding peak UV hours (10 AM to 4 PM) significantly reduces exposure to harmful radiation
- Seeking shade during outdoor activities represents a simple yet effective protective measure
- Regular skin self-examinations enable early detection of new or changing lesions
The implementation of these strategies requires consistent patient education and reinforcement. Healthcare providers play a crucial role in helping patients understand the long-term benefits of preventive measures and the importance of maintaining protective habits throughout their lives.
The Path Forward
While Actinic Keratosis presents ongoing challenges, modern dermatological approaches offer increasingly sophisticated solutions for both treatment and management. Success in controlling this condition relies on three key pillars: early detection, appropriate intervention, and consistent preventive measures. Regular dermatological consultations remain fundamental to monitoring progression and adjusting treatment strategies as needed.
The dynamic nature of AK management requires ongoing vigilance and adaptation of treatment approaches. As our understanding of the condition continues to evolve, new therapeutic options emerge, offering hope for improved outcomes and more targeted interventions.
Remember that protecting your skin from UV damage serves as the cornerstone of prevention. If you notice suspicious skin changes, particularly in sun-exposed areas, consulting a dermatologist promptly ensures proper evaluation and care. Through understanding, vigilance, and appropriate medical intervention, individuals can effectively manage this common precancerous condition while maintaining optimal skin health. The journey to skin health is continuous, but with proper medical guidance and patient commitment, successful management of Actinic Keratosis is achievable.