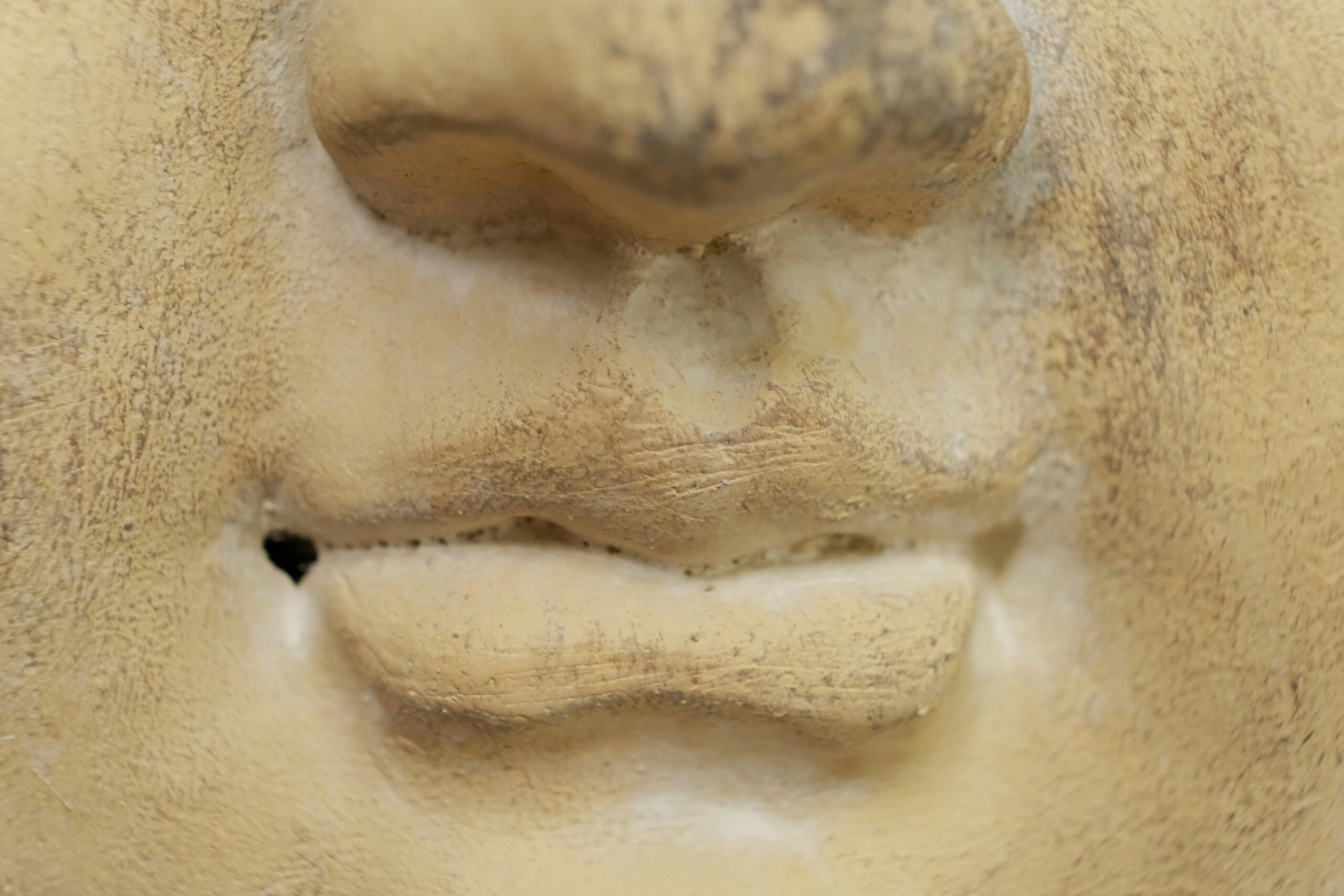
Facial psoriasis refers to a chronic skin condition in which the face is affected by one or more persistent, thickened, red, and dry patches.
Psoriasis is a common chronic inflammatory skin disease that may affect skin anywhere. The face is affected in half of the patients who have psoriasis. Usually, facial psoriasis is mild, but occasionally it can be very extensive at sites of the forehead, neck, hairline, ears, and facial skin.
It is extremely rare for individuals to have only facial psoriasis. A lot of patients also have scalp psoriasis and they may even have moderate to severe psoriasis at other body sites.
Patients with psoriasis often suffer from various psychosocial problems due to having red and scaly patches, or plaques on highly visible sites.
Facial involvement can be challenging to treat because facial skin is more thin and sensitive for regular therapeutic treatments.
Facial psoriasis has a wide range of clinical presentations. However, specialists have outlined three main subtypes: hairline psoriasis, sebo-psoriasis, and true facial psoriasis.
Hairline psoriasis is the extension of scalp psoriasis that goes beyond the hairline onto facial skin. Plaques appear bright red and thickened as well as have white scales.
In sebo-psoriasis, there is a patchy involvement of the hairline. Eyelids, eyebrows, nasolabial folds, and beard areas are usually affected. The plaques appear salmon-pink and thick with a bran-like scale. Sebo-psoriasis is usually associated with patchy or diffuse scalp psoriasis.
In true facial psoriasis, the plaques appear as sharply demarcated, red, and scaly. Plaques tend to be symmetrical. Any part of the face may be affected. True facial psoriasis is associated with psoriasis at other body sites, such as the scalp, ears, knees, and elbows.
Facial psoriasis has two distinct symptoms. The first symptom is the presence of mild to intense itch. The second symptom is soreness and skin sensitivity, which are usually mild.
The causes of facial psoriasis and psoriasis, in general, are the same. Psoriasis is associated with inappropriate immune system activation that results in increased proliferation and inflammation of skin cells. Psoriasis can have a genetic predisposition; however, environmental factors can also aggravate this skin condition. The environmental factors include infection, stress, and medications. Ultraviolet (UV) radiation, skin flora (e.g. yeast Malassezia), and smoking can aggravate facial psoriasis.
There is no cure for facial psoriasis; however, satisfactory control of the disease is possible for the majority of patients who use topical therapy.
General skincare involves using moisturizers, gentle non-soap cleansers, and sunscreens.
Topical steroids with mild or moderate strength help to reduce inflammation and relieve itching. The associated side effects of corticosteroids limit the potency and duration of use on the face. These include the following: easy bruising and tearing of skin; think and transparent skin, especially if eyelids are treated; periorificial dermatitis; telangiectasia; and possible increase of hair growth.
The topical tacrolimus ointment and calcineurin inhibitors pimecrolimus cream can be prescribed for facial psoriasis, especially eyelids. This treatment method tends to be effective and efficient.
Sun exposure or prescribed phototherapy is another effective method for treating facial psoriasis.
Severe facial psoriasis can sometimes be treated with tablets or injections like biologic agents, acitretin, cyclosporine, apremilast or methotrexate.
Facial psoriasis tends to persist. Its severity may vary with seasons, stress levels, and other factors.
Centre for Medical and Surgical Dermatology offers unique and personalized facial psoriasis treatment options for each patient.
For more information about psoriasis in general, visit the following link:
For World Psoriasis Day, visit the following link: