Melanoma represents one of the most aggressive forms of skin cancer, developing from the uncontrolled proliferation of melanocytes – the specialized cells responsible for producing skin pigment. Like a silent infiltrator, this formidable cancer can emerge from seemingly innocent skin changes, making vigilance and understanding crucial for every individual. This comprehensive guide explores the complexities of melanoma, its risk factors, early detection methods, and the critical importance of timely intervention.
Understanding Melanoma
At its core, melanoma is a malignant transformation of melanocytes, the cells that produce melanin – our body’s natural pigment. Think of melanocytes as tiny factories producing the protective coloring that shields our skin from harmful radiation. When these cellular factories malfunction, the result can be catastrophic. While other forms of skin cancer exist, melanoma stands apart due to its aggressive nature and potential for rapid spread to other body systems, much like an invasive species taking over new territory. The complexity of this cancer lies in its ability to develop virtually anywhere melanocytes are present, not just in sun-exposed areas.
Epidemiology and Risk Profile
Melanoma can affect individuals across diverse age groups, though certain populations face elevated risk levels. Like a complex tapestry, the risk factors for melanoma weave together genetic predisposition, environmental exposure, and individual characteristics. Understanding these risk factors proves crucial for prevention and early detection:
Primary Risk Factors:
Each risk factor represents a piece of the melanoma puzzle, contributing to an individual’s overall susceptibility:
- Age: Risk increases with advancing age, though young adults are increasingly affected. Like rings in a tree trunk, each year of life can bring accumulated cellular damage that may trigger melanoma development.
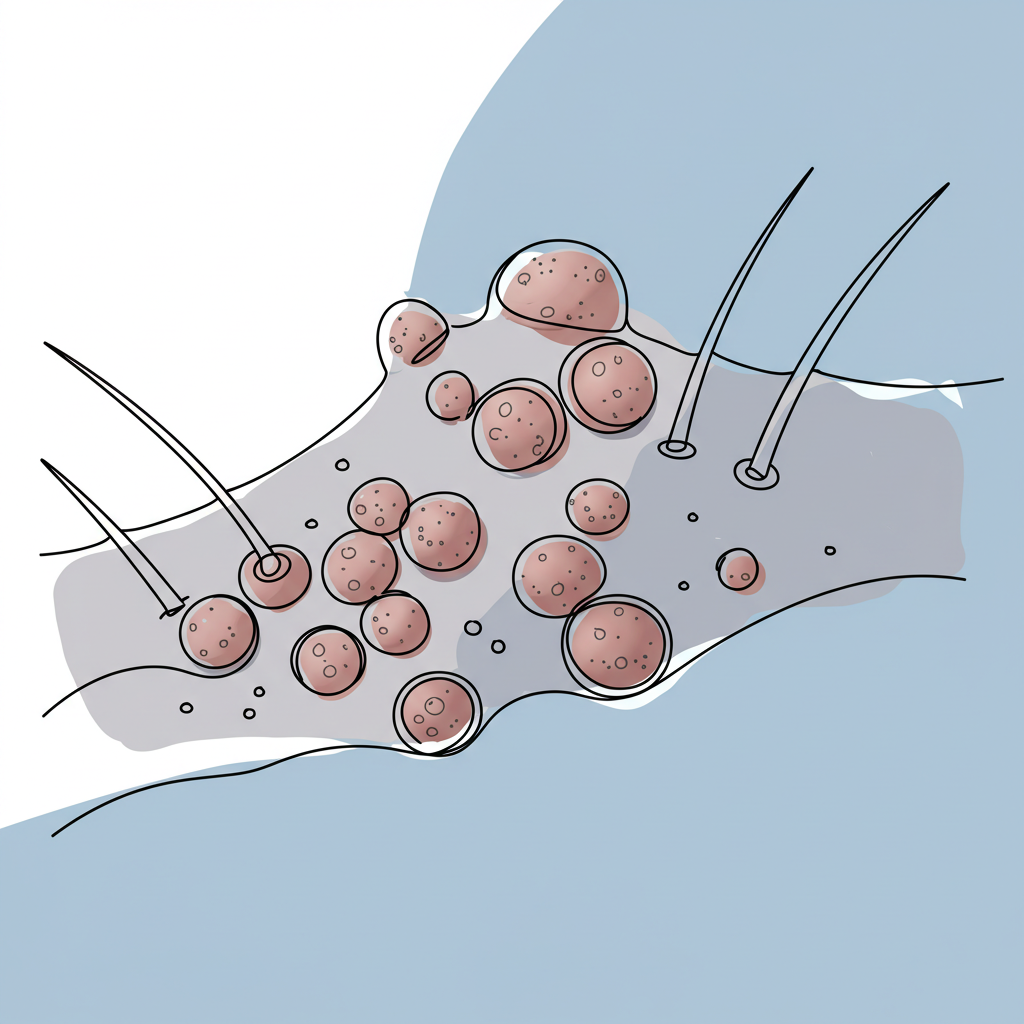
- Melanocytic Naevi: Multiple moles or atypical naevi significantly elevate risk, acting like potential launching pads for cancerous transformation.
- Genetic Predisposition: Family history plays a crucial role in susceptibility, passing down genetic vulnerabilities like inherited traits.
- Skin Type: Fair-skinned individuals face higher risk due to reduced natural UV protection, their skin lacking the melanin shield that darker-skinned individuals possess.
- Medical Conditions: Conditions like Parkinson’s disease correlate with increased melanoma risk, suggesting complex interactions between various bodily systems.
Additional Contributing Factors:
Understanding melanoma risk requires examining both direct and indirect influences that can affect cellular behavior and DNA damage:
- UV Exposure: Both natural and artificial UV radiation can trigger melanoma development. Like repeated blows to a defensive wall, each UV exposure event has the potential to damage cellular DNA and initiate cancerous changes.
- Previous Skin Cancer: History of any skin cancer increases melanoma risk, much like a warning signal indicating vulnerable skin tissue.
- Immune Status: Compromised immune systems may facilitate melanoma development, as the body’s natural defense mechanisms become less effective at identifying and eliminating abnormal cells.
Clinical Presentation
Melanoma manifests through various presentations, creating a spectrum of appearances that demands careful attention and regular monitoring. Like a chameleon of cancers, its ability to present in different ways makes vigilant skin monitoring essential. Key characteristics include:
Primary Signs:
The visual manifestations of melanoma often tell a story of cellular transformation, revealed through distinct physical changes:
- Morphological Changes: Progressive alterations in existing moles or new lesion development, similar to watching a photograph slowly distort over time
- Color Variations: Diverse pigmentation patterns emerge like an artist’s palette gone wrong, including:
- Deep black regions, reminiscent of ink spots
- Dark brown areas, varying in intensity
- Blue undertones, suggesting deep penetration
- Red components, indicating vascular changes
- Tan sections, blending with normal skin
The ABCDE Rule for Melanoma Detection:
This crucial diagnostic framework serves as a reliable compass for both healthcare providers and patients, guiding the evaluation of suspicious lesions:
- Asymmetry: Irregular shape with unmatched halves, like a butterfly with mismatched wings
- Border: Uneven or notched edges, resembling a coastline’s irregular pattern
- Color: Multiple colors or unusual pigmentation, creating a mottled appearance
- Diameter: Usually larger than 6mm (pencil eraser size), though early detection may reveal smaller lesions
- Evolution: Changes in size, shape, or color over time, documenting the lesion’s journey
Anatomical Distribution
Melanoma demonstrates remarkable versatility in its location, infiltrating various body systems with concerning adaptability:
- Cutaneous Sites: Can develop anywhere on the skin surface, from sun-kissed shoulders to hidden spaces between toes
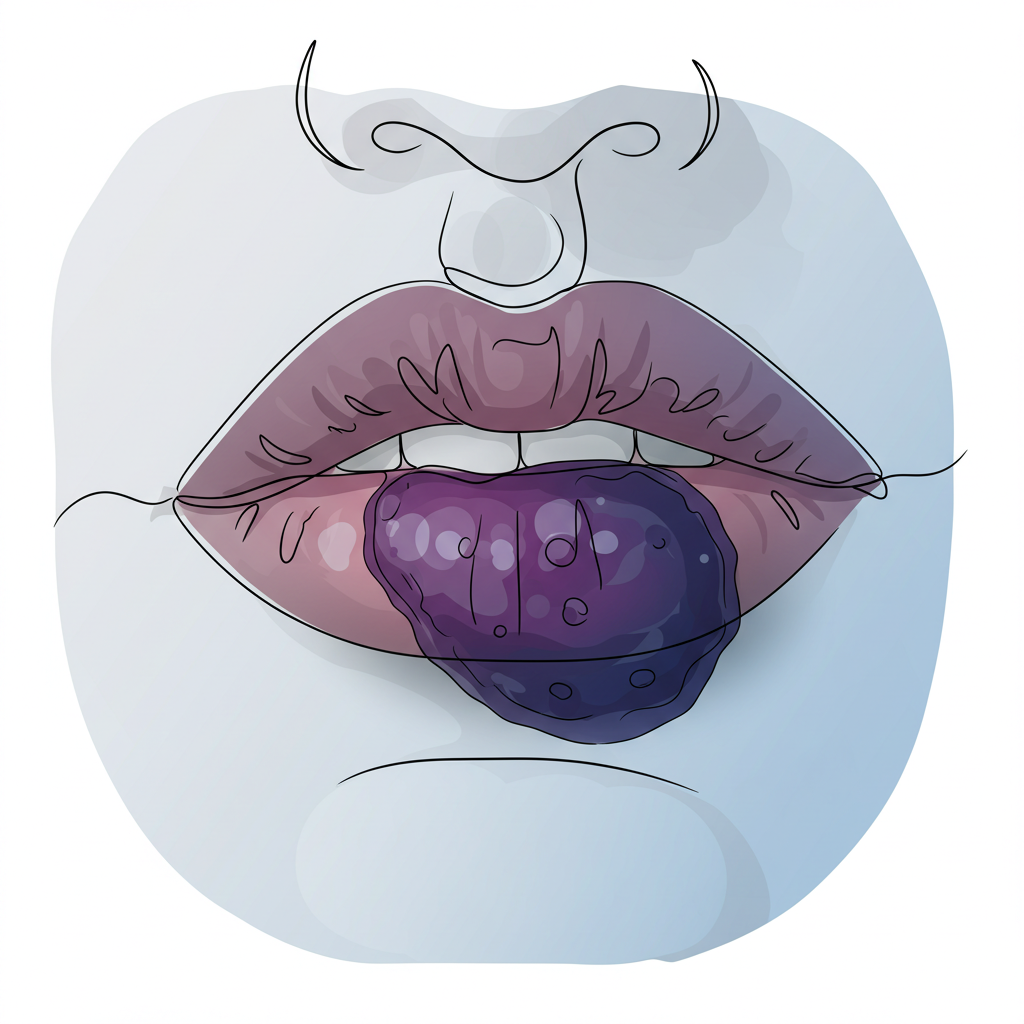
- Mucosal Surfaces: May affect mouth, nasal passages, or genital areas, areas often overlooked during skin examinations
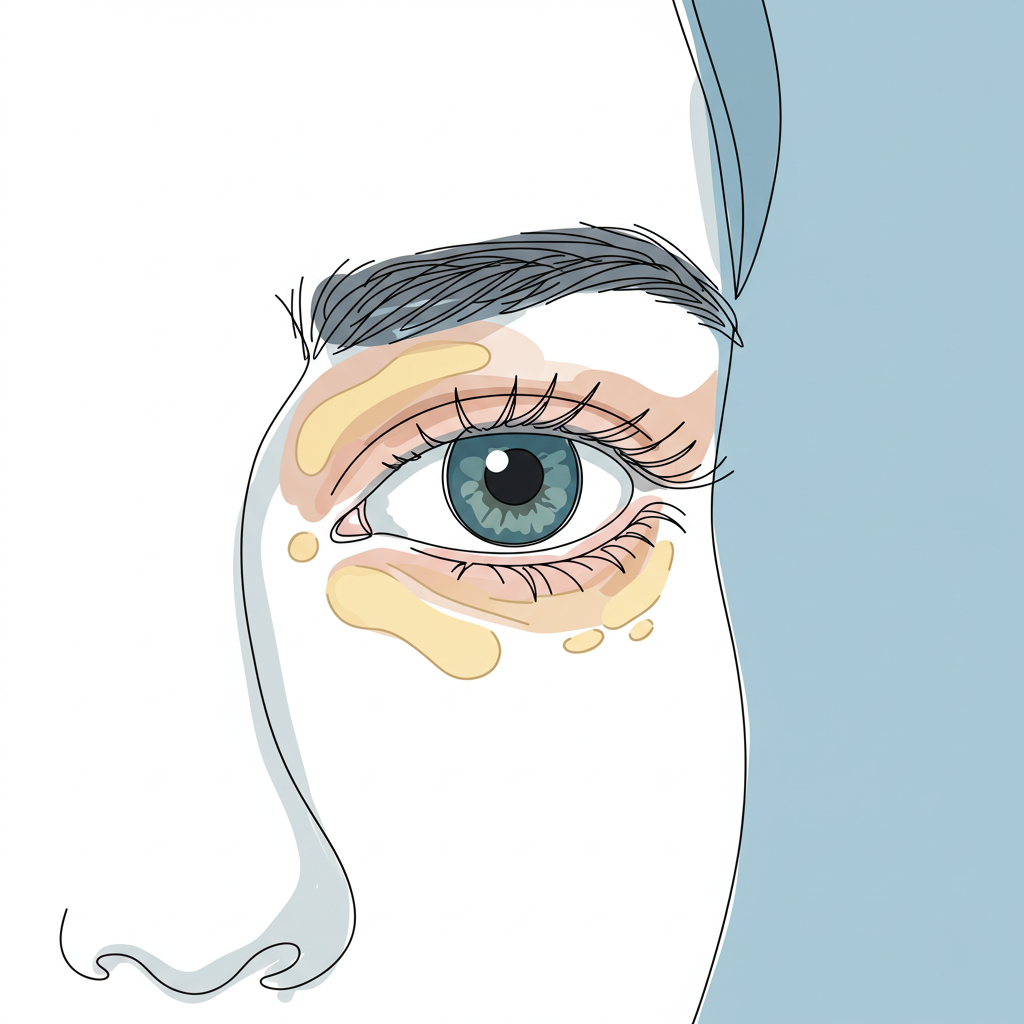
- Ocular Involvement: Can develop within the eye’s structures, requiring specialized detection methods
- Neural Tissue: Rare cases of primary brain melanoma exist, highlighting the cancer’s ability to emerge in unexpected locations
Clinical Features
The progression of melanoma often follows a predictable pattern, though variations exist, much like chapters in an unfolding story:
Early Signs:
Early recognition offers the greatest opportunity for successful intervention:
- Visual Changes: Unusual appearance of new or existing skin lesions, often the first chapter in melanoma’s development
- Surface Changes: Development of irregular texture or elevation, like topographical changes on a miniature scale
- Sensory Symptoms: Potential itching or discomfort, serving as early warning signals
Advanced Features:
The progression of melanoma into advanced stages manifests through increasingly concerning changes that demand immediate medical attention:
- Physical Changes: Continued growth and morphological alterations become more pronounced, as the lesion evolves beyond its original boundaries. This progression may include vertical growth into deeper skin layers, significantly impacting prognosis.
- Bleeding: Spontaneous bleeding or easy bruising of the lesion indicates significant structural changes within the tumor. This symptom often reflects the development of fragile blood vessels and compromised tissue integrity.
- Systemic Symptoms: As melanoma advances, patients may experience constitutional symptoms such as fatigue, unexplained weight loss, and declining performance status, signaling the cancer’s broader impact on the body.
Prevention Strategies
While melanoma’s aggressive nature demands respect, a comprehensive prevention strategy can significantly reduce risk. Like building a fortress against invasion, multiple layers of protection offer the best defense:
1. Sun Protection:
The cornerstone of melanoma prevention lies in sophisticated UV defense strategies:
- Regular use of broad-spectrum sunscreen with minimum SPF 30, reapplied every two hours during sun exposure
- Protective clothing coverage, including UV-resistant fabrics and wide-brimmed hats
- Strategic avoidance of peak UV exposure hours, typically between 10 AM and 4 PM
- Understanding the UV index and adjusting outdoor activities accordingly
2. Skin Monitoring:
Vigilant surveillance serves as an early warning system:
- Monthly self-examinations using proper lighting and mirrors
- Professional skin checks at intervals determined by risk factors
- Photographic documentation of existing moles to track changes over time
- Special attention to high-risk areas like the back, scalp, and between toes
3. Risk Management:
Proactive risk reduction requires a comprehensive approach:
- Prompt evaluation and removal of suspicious lesions by qualified healthcare providers
- Genetic counseling for individuals with strong family history
- Lifestyle modifications including smoking cessation and maintaining healthy weight
- Regular medical follow-up based on individual risk assessment
Conclusion
Melanoma represents a formidable adversary in the landscape of skin cancer, demanding respect, understanding, and vigilant monitoring. Like sentinels guarding against invasion, healthcare providers and patients must work together to identify and address potential threats early. Understanding its characteristics, risk factors, and warning signs empowers individuals to take proactive steps in prevention and early detection.
The journey of melanoma management exemplifies the critical intersection of medical science and patient engagement. Through careful observation, timely intervention, and comprehensive prevention strategies, the impact of this aggressive cancer can be minimized. Regular skin examinations and prompt medical consultation for suspicious lesions remain cornerstone strategies in managing this serious form of skin cancer.