Electrosurgery has become a cornerstone in dermatological practices, widely utilized for its effectiveness in achieving haemostasis and eliminating abnormal skin growth. This method leverages high-frequency, alternating electric currents to generate heat, making it a versatile and precise tool in skin treatments. Below, we explore the mechanics, applications, and considerations associated with electrosurgery in dermatology.
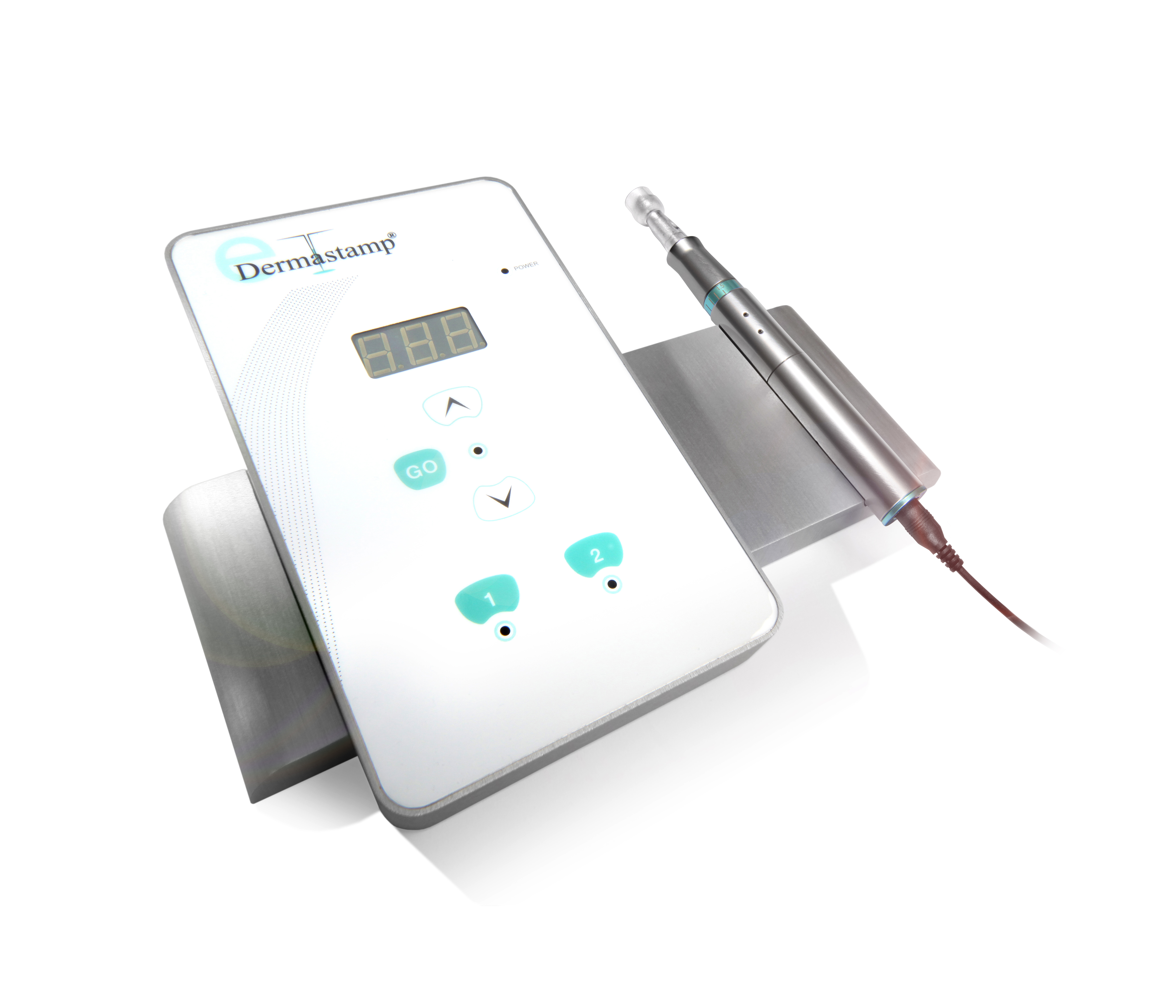
Electrosurgery operates by passing electric currents ranging from 200 to 10,000 volts through the skin, producing heat to coagulate or destroy tissue. The equipment typically includes a power supply and a handpiece equipped with one or more electrodes. The device’s operation is controlled via a switch on the handpiece or a foot pedal, allowing clinicians to adjust parameters as needed.
However, the terminology surrounding electrosurgery can sometimes cause confusion. While the overarching aim of the procedure is cauterization (a term derived from the Latin for “branding”), it’s essential to distinguish between electrosurgery and other related techniques. For instance, true electrosurgery involves alternating current, while “electrocautery” typically refers to the use of direct current to heat a probe—more accurately termed thermocautery. Similarly, diathermy, a term often misapplied to electrosurgery, relies on molecular dipole rotation in high-frequency fields and is fundamentally different.
Electrosurgery encompasses several specialized techniques, each tailored to specific clinical needs:
1. Electrofulguration: Produces sparks to dehydrate and carbonize superficial tissues, commonly used for treating skin tags, warts, and seborrhoeic keratoses. The electrode remains slightly above the skin, generating an electric arc.
2. Electrodesiccation: Directly contacts the skin, causing dehydration of surface and subdermal tissues. It is suitable for lesions such as syringomas, milia, or sebaceous hyperplasia and is also used for hair removal and fine blood vessel treatment.
3. Electrocoagulation: Targets deeper tissue, achieving haemostasis by coagulating blood vessels. This technique is indispensable for treating skin cancers and vascular conditions like pyogenic granulomas.
4. Electrosection: Combines cutting and coagulation, allowing for the excision of vascular lesions with minimal thermal damage to surrounding tissue. It is frequently employed in the removal of benign moles, skin tags, or seborrhoeic keratoses.
5. Thermocautery: Utilizes direct current to heat a probe, which transfers thermal energy to the tissue. Unlike other forms of electrosurgery, the treating electrode remains cold, making this technique ideal for patients with implanted cardiac devices.
6. Radiofrequency Devices: Operate at extremely high frequencies (>1,500 kHz), providing precision in cutting with minimal collateral damage. These devices are often preferred for non-ablative skin tightening and other cosmetic applications.
Electrosurgery can be categorized into monoterminal, monopolar, and bipolar modalities, depending on the configuration of electrodes:
– Monoterminal Electrosurgery: Features a single electrode and does not require an indifferent electrode.
– Monopolar Electrosurgery: Uses a pointed probe to deliver current, with an indifferent electrode placed on the patient to complete the circuit. It is widely used but requires careful grounding to prevent burns.
– Bipolar Electrosurgery: Employs forceps with active and indifferent electrodes on each tine. This technique confines the current to the tissue grasped by the forceps, minimizing risks for patients with implanted cardiac devices.
Electrosurgery is indispensable in treating various dermatological conditions. Electrofulguration and electrodesiccation are ideal for superficial lesions like warts and seborrhoeic keratoses. Deeper tissue destruction is achieved through electrocoagulation, suitable for vascular lesions and cancerous growths. Meanwhile, electrosection provides precision in excising lesions with minimal scarring.
Despite its advantages, electrosurgery carries risks, including burns, electric shocks, infection transmission, and exposure to toxic gases. Proper precautions, such as using smoke evacuators, insulated tables, and personal protective equipment, are essential to safeguard both patients and practitioners.
Patients with implanted pacemakers or defibrillators require particular attention during electrosurgical procedures. The use of bipolar devices or thermocautery is recommended to prevent interference with the cardiac device. In complex cases, collaboration with a cardiologist is crucial to ensure patient safety.
Modern electrosurgical tools, like the Conmed Hyfrecator®, offer enhanced precision and versatility. These devices support a range of electrodes tailored for specific applications, from haemostasis to lesion excision. Innovations such as Teflon-coated tips and smoke evacuation systems further improve safety and efficiency, cementing electrosurgery’s role as a mainstay in dermatological practice.
In conclusion, electrosurgery is a highly effective method for treating a range of dermatological conditions, from benign growths to malignancies. With proper technique and adherence to safety protocols, it offers excellent outcomes with minimal risks, making it a valuable tool in modern dermatology.